
- Articles
Longevity and compression of morbidity from a neuroscience perspective: Do we have a duty to die by a certain age?
Abstract — The search for longevity, if not for immortality itself, has been as old as recorded history. The great strides made in the standard of living and the advances in scientific medicine, have resulted in unprecedented increases in longevity, concomitant with improved quality of life. Thanks to medical progress senior citizens, particularly octogenarians, have become the fastest growing segment of the population and the number of centenarians is increasing, even though in the last two decades, spurred by the bioethics movement, the priority assigned to the prolongation of lifespan has taken a back seat to the containment of health care costs. This article describes what individuals can do to lead healthy lifestyles and increase longevity, concomitant with preservation of quality of life until the very end of life—as postulated by Dr. James F. Fries’ hypothesis of the compression of morbidity. This review article investigates the contention of bioethicist Dr. Ezekiel Emanuel that Fries’ theory is a “fantasy” and not a realistic possibility. In this context recent advances in neurobiology, epigenetics, and aging are described, and the hypothesis of the compression of morbidity re‑examined. We find that people are not only living longer but are remaining healthier. Recent studies suggest that brain plasticity develops and potential neurogenesis occurs in those individuals who continue to be mentally and physically active allowing them to thrive well into old age. Controlled studies as well as Medicare spending data strongly corroborate Fries’ predictions and support my conclusion that compression of morbidity should be upgraded from a hypothesis to a theory. Lastly, leisure in association with or without retirement is discussed and suggestions are made as to how to use this time to remain intellectually sharp and physically vigorous until the very end of life.

The search for immortality has almost been as old as recorded history. In fact the Epic of Gilgamesh, the oldest of the great extant works of literature, concerns man’s eternal search for immortality. The main figure, Gilgamesh, the king of the Sumerian city of Uruk in Mesopotamia, is a demigod of superhuman strength who lived between 2800 and 2500 B.C. [Figure 1]. But despite his heroic feats, Gilgamesh has a weakness. He is mortal and seeing death all around him, taking the lives of even his companions, he becomes obsessed with cheating death. Seeking immortality, Gilgamesh goes in search of Utnapishtim, an old survivor of the Great Deluge, probably the same cataclysmic event as mentioned in the Biblical account of Noah and the Flood. Supposedly, Utnapishtim possessed the secret of eternal life. It is the adventures of our hero searching for an elixir of immortality, which is the grand subject of the Epic of Gilgamesh.[29]
A more recent account of the search for eternal life is that of the historic Spanish conquistador, Juan Ponce de León (c. 1460-1521), who explored Florida in 1513. According to a legend told by the Indians, there existed a “fountain of youth” hidden in the swampy marshes of the exotic Florida peninsula. In pursuit of this elusive fountain, Ponce de León went on a fruitless quest. Assailed by hostile Indians and unsuccessful in his first attempt to find the secret, he returned empty-handed to Cuba. On a return trip to Florida in 1521, Ponce de León was attacked by bellicose Indians near Tampa Bay and mortally wounded. He never found the legendary fountain and the secret to man’s immortality was never discovered.[24]
The elixir of immortality may lie, not in secrets held by mythic heroes of antediluvian times or in fountains of youth hidden in the marshy swamps of Florida, but in science and in the pursuit of healthy lifestyles. The great strides made in hygiene and sanitation, the remarkable improvements in the standard of living, the advances in scientific medicine, and the success achieved with alterations in lifestyles have resulted in unprecedented increases in longevity, concomitant with improved quality of life. Those interested in reading about the great events in medical history in the unprecedented 19th and 20th centuries that made these advances possible are invited to read further on this topic.[22-24]
The New Bioethics Movement: Should we Live a Long and Healthy Life or do we Have a Duty to Die at Age 75?
Thanks to medical progress, senior citizens, particularly octogenarians, have become the fastest growing segment of our population, even though in the past two and a half decades, the priority assigned to the prolongation of lifespan has silently taken a backseat to other items in health care policy, chiefly the containment of health care costs. Toward this utilitarian goal, politically feasible methods for the rationing of medical care under the rubric of the concept of the “rational allocation of finite and scarce health resources,” have been sought. In this context, the concept and pursuit of longevity (from the Latin longaevitas, meaning “long-lived”) has been almost abandoned for the more contemporary concepts of “useful lifespan,” “the duty to die,” “assisted suicide,” and, its more socially palatable term, “the right to die”—terms all propounded by various factions of the bioethics movement.[2,15,20,21]
Nevertheless, the dramatic extension of lifespan, closely associated with improvement in the quality of later life, is welcomed news for the remarkable generation of “baby boomers,” as well as succeeding generations who have much to gain from advances in longevity with improved quality of life as they age in the first half of the 21st century.[20,24,33]
Nevertheless, as intimated in preceding paragraphs, a clash of alternative ethical philosophies of medicine is taking place as to the direction society should take in the pursuit of the proper allocation of health resources. Bioethicists in general subscribe to a collectivist (socialist) and utilitarian philosophy of rationing health care and redistributing medical resources among those younger and “useful” members of society. Dr. Ezekiel Emanuel has written that longevity should be limited to age 75. After reaching that age, Emanuel—who incidentally is no crackpot but a respected bioethicist, one of the architects of ObamaCare and the Director of the Clinical Bioethics Department at the U.S. National Institutes of Health—claims life is a downhill spiral after age 75 and not worth living.[19] His celebrated thesis has been contravened in a previous editorial in Surgical Neurology International (SNI)[20] and will be further refuted in this review article. Nevertheless, today the views of leading bioethicists are consonant with those of Emanuel and although countered by a few traditional medical ethicists, the new bioethics movement holds sway in the hospitals and ethics boards of the United States and most Western nations [Figure 2].[2,15,18,20,21] In this context, in the United Kingdom, British pensioners are being denied life-saving operations and treatments within the National Health Service (NHS) because of age discrimination. This lethal prejudice against advancing age has been going on for years, but at long last the Royal College of Surgeons is beginning to speak against the practice. After age 75, which interestingly seems to be the inauspicious chronological age, no cholecystectomies, no knee replacements, and no mastectomies for breast cancer are performed, and patients are left to die in pain and without mobility.[18] Yet, the wind may be beginning to blow in the opposite direction and the future looks brighter. A movement toward reversal of this age discrimination seems to be on the horizon. In fact, the title of a British article reflects this optimism: “Longevity is here to stay—embrace it.” According to this article, “the Office for National Statistics predicts that about one in three babies born in the UK last year will live to celebrate their 100th birthday [Figure 3], and the total number of centenarians is projected to rise from 14,000 in 2013 to 111,000 in 2037.”[33]
Leading a Healthy Lifestyle Improves Longevity and Preserves the Quality of Life
The search for useful drugs and therapies to ameliorate the human condition in illness and advancing age continues. The debate as to health priorities goes on. Scientific research continues. In the meantime, there are steps we can take to lead healthier lives. There is evidence long-term memory, for example, can be improved with 20 minutes of moderately strenuous exercise. It is postulated chemicals that improve memory are released with sustained moderate physical exertion. Aerobic, as well as resistance exercises, have been shown to improve memory as physiologic responses to exercise.[46] A balanced diet may not only help maintain normal glucose and vitamin levels but the addition of vegetable and fruit nutrients (i.e. containing choline and flavonoids) may also help in memory retention. The time-tested advice offered by our parents and grandparents was sound and correct: Most people need 7-8 hours of sleep for healthy living, proper concentration, and proper memory retention. As we age we do have problems with recollection, particularly short-term memory. Lack of sleep impairs memory, and sleep deprivation causes a distortion of memory.[26]

There is much that individuals can do to eliminate premature death, increase their longevity, and preserve the quality of their lives in old age (i.e. compression of morbidity). Many of us can age gracefully, remain healthy and preserve quality of life, if we follow the 10 basic rules I consider essential: (1) Control of body weight via proper diet and calorie count, preferably via three small, balanced meals a day [Figure 4]; (2) No tobacco or cigarette smoking; (3) Attention must be paid to cholesterol levels and the maintenance of the proper ratio of the high-density (HDL) and low-density (LDL) lipoproteins that transport cholesterol in the blood; (4) Exercise daily (or at least every other day); (5) Avoid excessive sun exposure (and harmful solar radiation); (6) Attention must be paid to individual requirements for vitamin, mineral, and nutritional supplementation; (7) Medical examination should be conducted at intervals and medical advice by the personal physician followed regarding diagnostic tests, recommended therapies, nutritional needs, medications prescribed, and genetic counseling when advisable; (8) Alcohol should be consumed in moderation (consumption of one or two servings of red wine daily may in fact be beneficial); (9) Frequent checks with maintenance of proper blood pressure control; (10) Preservation of mental health, positive attitude, and proper use of leisure time. Additionally, awareness of family history and genetic predisposition to certain diseases is imperative for preventive medical intervention prior to the onset of disease.
How Exactly do we Follow the Ten Basic Rules Leading to Healthy Lifestyles?
As further explanation, let us expound on the 10 basic points as follows: Point 1, restriction in caloric intake, prevents obesity as well as helps prevent diabetes and high blood pressure. A proper diet consists of low saturated fats and high quality proteins; limiting salt intake; limiting simple sugars and incorporating instead whole grains rich in fiber. Diets should be imperatively watched in patients with suspected or diagnosed diabetes, obesity, hypertension, and hyperlipidemia. Point 2 is self-explanatory. The dangers of smoking have been well-publicized, and consequently smoking rates are falling worldwide with a concomitant decrease in atherosclerotic cardiovascular disease. Point 3 concerns the lipoprotein molecules that carry cholesterol and other lipids in the blood. HDL called the “good” cholesterol because high levels of this factor (e.g. 60 mg/dl) are associated with decreased incidence of atherosclerotic cardiovascular disease. HDL extracts excess cholesterol from the walls of blood vessels and carries it to the liver, where it is metabolized and the breakdown products secreted in the bile. In contrast, LDL circulates the “bad” cholesterol, and is associated with an increased risk of myocardial infarction and cerebrovascular disease. Thus, the ratio of these two factors is an important determinant of atherosclerotic cardiovascular disease, and morbidity and mortality as we age.
Point 4 reminds us to perform mild-to-moderate exercises daily to help maintain proper body weight as well as to keep us fit. A combination of aerobic activities to increase heart rate, as well as moderate weight-bearing and muscles strengthening exercises have been recommended; stair climbing is an excellent exercise that combines these features. Moderate exercise should be preceded by mild stretching to reduce stiffness and increase flexibility. I recommend exercising 4-5 times per week for 45-60 minutes. Dr. Russell L. Blaylock, a neurosurgeon and President of Advanced Nutritional Concepts and Theoretical Neurosciences Research, refrains from recommending vigorous exercise, particularly in the elderly.[8] We will have more to say about physical activities and exercise later. Suffice to say, patients should check with their physicians before beginning any exercise program. Point 5, excessive sun exposure should be avoided with protective clothing and routine sunscreen application. I recommend water resistant, sunscreen lotion, broad spectrum SPF 45 or greater, applied daily in the morning. Solar radiation causes a variety of skin cancers including malignant melanoma. It also causes damage and accelerated aging in the skin. Avoidance of sun exposure, though, results in iatrogenic depletion of Vitamin D that needs to be supplemented orally with milk products and Vitamin D-containing calcium tablets.
Point 6, multi-vitamins, natural plant products, and other nutritional supplementation have also been strongly advocated by both Drs. Blaylock and Joseph C. Maroon, a neurosurgeon at the University of Pittsburgh, in the context of neutralizing harmful free radicals, oxidation, protection against immunoexcitotoxicity that plays a major role in the development of many neurodegenerative diseases of aging, and correcting nutritional deficiencies.[9,11,14,36] In the same vein, certain drugs and food additives that cause neurotoxicity, such as excitotoxins should be avoided. Blaylock also advises avoidance of exposure to man-made toxins (e.g. harmful chemicals like herbicides and pesticides) and protection against environmental factors that cause inflammation, reduce immunity, and damage to various organs systems.[6,7,13,14] Points 7 through 9, referring to the necessity of following medical advise, alcohol consumption in moderation, and control of blood pressure, are self-explanatory. Allow me to just comment that red wine has been shown to lower the risk of atherosclerotic heart disease, probably by direct action of flavonoids or by their action in preventing oxidation of HDL.[10,36] And let us recall that hypertension, “the silent killer,” is a major cause of myocardial infarction, strokes, and arteriosclerosis; it needs to be treated aggressively. Point 10 refers to mental health and the need to maintain a positive attitude, the best possible attitude given the vicissitudes of life and personal circumstances. It also means coming to terms with aging in a positive light, whether one pursues the same active endeavors that continue to bring forth pleasure and fulfillment,[3] or whether one changes course, slowing down and planning a leisurely retirement, as with Voltaire’s famous counsel, “cultivate your garden.” The important thing is to maintain a positive attitude and remain active.[3,20,35,36] The great Aristotle (384-322 B.C.) wrote of the importance of leisure in intellectual pursuits, the enjoyment of life’s pleasures in moderation—in short pursuing knowledge and happiness for their own sake.[1] Toward the conclusion of this paper, in fact, I return and amplify on this Aristotelian notion of the “good life.”
In addition to the 10 points, I also alluded to genetic predisposition to certain diseases and mentioned genetic counseling under Point 7. We must become knowledgeable of our family history and our genetic legacy predisposing us to certain ailments and conditions. It has been estimated that 35% of susceptibility to disease and premature death is determined by our DNA. There is little we can do in this area. At present, gene manipulation to modify or delete the “bad” genes that shorten lifespan is an area of active genetic research. The quest for human “longevity genes” has had unfortunately very little success. Blaylock quotes Dr. James Vaupel of the Max Planck Institute as asserting that “only 25% of the variation in maximum lifespan can be attributed to genetics.”[12] I suspect 35% is closer to the mark. As far as defective or “bad genes,” one group of genes that have been singled out as having a “major impact on longevity” is the group of apolipoprotein E genes (APOE). APOE are produced by astrocytes and transport cholesterol to neurons and microglia. Of these, the APOE e4 allele variant is thought to increase the risk of several degenerative disorders, including Alzheimer’s disease (with amyloid plaque formation), atherosclerosis, and posttraumatic encephalopathy.[12,30,42] Another defective or “bad gene” is JAK (i.e. the Janus Kinase system; named after the Roman god of two faces, representing the beginning and ending of life). This gene codes for the kinase enzymes controlling phosphorylation. The JAK2 is, for example, a mutated gene that codes for a defective protein that can precipitate blood coagulopathies, myeloproliferative, and/or myelodysplastic disorders, in previously healthy people with no previously known genetic abnormalities. The JAK2 mutated gene has also been identified as one of the oncogenes linked to the development of some leukemias and lymphomas.[34] Fortunately Janus kinase inhibitor drugs are under development and, as previously mentioned, defective genes appear to play only a limited role in shortening life expectancy.
Preventive therapies, such as prophylactic mastectomies and terminations of pregnancies (following abnormal amniocentesis and the presence of genetic defects in the fetus), are currently being done for high-risk patients with strong family histories or with documented genetic predisposition to certain malignant diseases. There is still much we can do for the other 65% of diseases, as I have outlined, where genetics seem to play a minor role.
Is the Seeking of ‘The American Immortal’ a Real, Obsessional Fantasy?
Bioethicists claim Americans are too preoccupied, obsessed, with finding ways of prolonging life when they should be making way for the younger generation. Americans may want to live longer, but they want this blessing with a concomitant preservation of health and quality of life. In the aforementioned article, Dr. Ezekiel Emanuel decries the yearning of what he called “the American immortal,” futile efforts to “cheat death and prolong life as long as possible.”[19] Supposedly, Americans desperately want to believe in the “compression of morbidity” theory developed by Dr. James F. Fries, professor of medicine emeritus at Stanford University. Emanuel explains, “this theory postulates that as we extend our life spans into the 80s and 90s, we will be living healthier lives—more time before we have disabilities, and fewer disabilities overall. The claim is that with longer life, an ever smaller proportion of our lives will be spent in a state of decline.”[19] To Emanuel, this futile and erroneous theory, “tells us exactly what we want to believe: That we will live longer lives and then abruptly die with hardly any aches, pains, or physical deterioration—the morbidity traditionally associated with growing old. It promises a kind of fountain of youth until the ever-receding time of death. It is this dream—or fantasy—that drives the American immortal and has fueled interest and investment in regenerative medicine and replacement organs.”[19]
Is the compression of morbidity hypothesis of Dr. Fries then a fantasy or a medical possibility? To answer this question we need to review Fries’ original paper and then ascertain if his hypothesis has been confirmed by other investigators and found in accordance with accumulating data. First, then, what is the term compression of morbidity? Let us define it as a public health hypothesis first propounded in 1980 by Dr. James F. Fries, who described it as: “Think about two points on a typical human lifespan, with the first point representing the time at which a person becomes chronically ill or disabled and the second point representing the time at which that person dies. Today, the time between those two points is about 20 years or so. During the early portion of those years, chronic disease or disability is minor, but increases nearer to the end of life. The idea behind compression of morbidity is to squeeze or compress the time horizon between the onset of chronic illness or disability and the time in which a person dies.”[27]
The concept came about in the course of Fries’ medical research into life expectancy. He found there is a finite number of cell doublings associated with different species’ lifespan (i.e. the Hayflick phenomenon). The number of doublings of human fibroblasts is approximately 50. The number of doublings of cells in a culture medium is specific for all species studied. Species with more doublings were noted to have longer longevity than species with less doublings. Fries also found another factor determining lifespan—i.e. organ reserve. The physiological capacity of vital organs, which he called organ reserve, in young adults is 4-10 times that required to sustain life. Loss of organ reserve with progressive dysfunction, as with increasing age or illness, disturbs the organism’s ability to maintain homeostasis, and results in natural death in the absence or presence of disease.[27]

Chronic diseases are ailments caused by progressive loss of organ reserve, such as congestive heart failure with loss of myocardial reserve, emphysema with loss of pulmonary capacity, etc. Chronic illnesses now account for 80% of all deaths and an even higher percentage of disability. Moreover, Fries postulated that the average length of life is increasing because of the elimination of premature death, particularly in the area of atherosclerotic cardiovascular diseases. This is taking place because of the advances in medicine, such as more effective surgery and treatment of hypertension, hyperlipidemia, diabetes, etc., as well as improved lifestyles, such as decrease in smoking rates, better diets, regular exercise, etc. Obviously there is room for even more improvement: We have a serious problem with obesity and many Americans still lead sedentary lifestyles, others engage in self-destructive behaviors.[25] Many Americans are seriously overweight, if not outright morbidly obese. Many people who should be walking and using stairs are instead riding motorized carts and climbing on elevators. Nevertheless, pointing out the positive elements, Fries posited “the amount of disability can decrease as morbidity is compressed into the shorter span between the increasing age of onset of disability and the fixed occurrence of death.”[27] Weight control and regular exercise can modify the process of aging and improve plasticity by increasing performance as we age [Figure 5]. To increase plasticity and improve organ reserve, Fries’ motto is “use it or lose it.” Maintenance of organ capacity requires repeated use, practice, self-expression, and individual autonomy—until the “terminal drop.” At the top of the list of health research projects, Fries lists “the ability to postpone chronic illness, to maintain vigor, and to slow social and psychologic involution.”[27]
Epigenetics and Gene Activation in Health and Disease
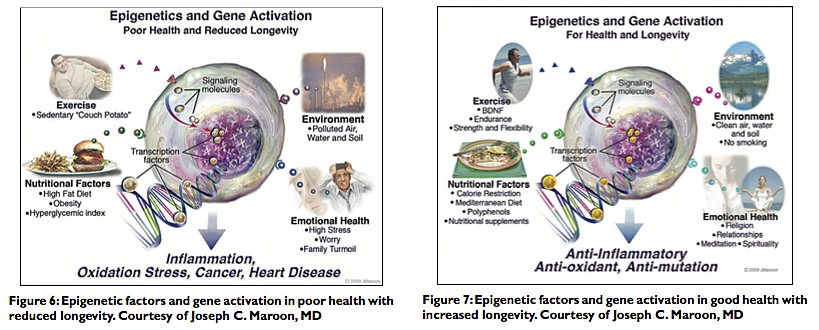
Epigenetic factors should also be considered in discussing life expectancy, health, and longevity. Epigenetics refers to activities, good or bad, such as the types of diets we consume and the exercises we perform, influencing gene expression. The choice of these activities in daily life affects gene activation with beneficial or unhealthy consequences. Maroon has written a remarkable book on this subject.[36] Figures 6 and 7 summarize the concept of how epigenetics affect gene activation, resulting in poor health and reduced longevity because of the activation of “bad” genes resulting in inflammation, oxidation, stress, cancer, or heart disease [Figure 6]. Activation of “good” genes, in contrast, results in good health and longevity because of anti-inflammatory, anti-oxidant, and anti-mutation stimulation [Figure 7].[35]
Remaining mentally and physically active are the most important things one can do to preserve health and improve longevity. Maroon affirms: “Exercise is also the best stimulant for brain-derived neurotrophic factor (BDNF), which increases neurogenesis, neuroplasticity, and synaptogenesis. To this end, I have continued a daily exercise regimen and also regularly compete in triathlons and other endurance events.”[35] Maroon also emphasizes, “the importance of prayer, meditation, strong family units, yoga, tai chi, biofeedback, and exercise—whatever works for the individual—to reduce stress and anxiety and decrease the overproduction of hormones and neurotransmitters that can become toxic.”[35] Individuals should avoid exposure to toxic chemicals and certain food additives such as excitotoxins[6,7] as well as chronic stress, which have been shown to cause the production of harmful free-radicals, oxidation of cellular tissues, and mutation in the human genome. Chronic stress also causes the deleterious release of cortisol that can also result in memory impairment, dehydration of the brain, chromosomal damage, and accumulation of abdominal fat.[35,36] For his part, Dr. James I. Ausman, professor of neurosurgery at UCLA and editor-in-chief of Surgical Neurology International (SNI) recommends vigorous mental activity and planning ahead with your spouse, as to learn and grow together, “That is what I have done by developing multiple careers in neurosurgery, becoming editor of a journal, and studying the challenges of aging and developing a consulting company and a television series on that subject, all with the joint efforts of my wife of 53 years, Carolyn.”[3]
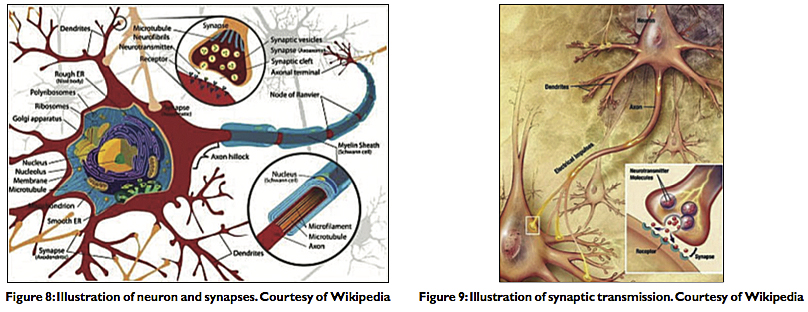
Under this heading, I should recapitulate that recent studies suggest that brain plasticity and neurogenesis allow individuals to continue to learn well beyond middle age into old age for those who remain mentally and physically active.[3-5,20,35,36,41] It may be that neurons and synapses continue to be generated with continued physical and intellectual activity [Figure 8]. There is evidence that neuroglia, neurons (i.e. neurogenesis), and their synapses (i.e. synaptogenesis) continue to be produced as a result of repeated physical exercise as well as continued intellectual activity even in older individuals. This may be the case because both physical and mental activities have been posited to stimulate the production of brain-derived neurotrophic factor (BNDF). BNDF is a protein in the neurotrophin family and a potent neurogenic factor, as such it supports neurons and synapses and encourages their growth [Figure 9]. BNDF has been shown to be active in the limbic system and cerebral and basal cortices, areas vital to learning, short- and long-term memory formation, cognition, and critical thinking.[32,47] The importance of physical and intellectual activity as we get older cannot then be overemphasized in postponing senescence and the arrival of death as long as possible.[20,27] Mental exercises (e.g. solving crossword puzzles) and active intellectual pursuits—such as reading, writing, and multilingualism—have been shown to not only prevent premature aging but also to postpone the onset on neurodegenerative disorders such as Alzheimer’s and Parkinson’s disease.[4,5,41]
Is True Extension of Longevity with ‘Compression of Morbidity’ a Feasible Reality?
Let us now return to Fries’ hypothesis. Compression of morbidity suggests that the onset of chronic infirmity can be postponed so that the hardship of chronic and debilitating illnesses as we get older can be compressed into a shorter period of life—until the finality of death. In contrast, bioethicists and government planners are concerned (and have convinced themselves) that the opposite is the case, and that as the American population ages they will become progressively infirm, utilize more medical care, increase health care costs, and consume larger portions of the national budget.[2,15,19,20,43]
While it is self-evident that life does not get easier or necessarily longer for all of us, Fries revealed with collected data and supporting graphs that Americans generally were not only living longer but were remaining healthier, even as they aged, up until close to the very end of their lives—the very essence of the compression of morbidity. As he explained, “adult vigor can be extended well into the ninth decade of life, with illness and disability compressed into a period that shortly precedes death.”[27] In 1998, Fries’ findings were in fact bolstered, his tentative hypothesis on the compression of morbidity tentatively confirmed in a study of 1700 University of Pennsylvania alumni followed over a period of 20 years. The participants were first surveyed in 1962 and then annually starting in 1986. The researchers found “not only do persons with better health habits live longer, but serious chronic illness and disability are also postponed and compressed into fewer years, improving quality of existence at the end of life.”[44] And so, it turns out that Fries’ hypothesis may not be a dream or fantasy—but a reality.
Fries hypothesis was further corroborated in 2002 in a study of 960 participants (average age 59): 537 members of a runners club and 423 community controls over a 12-year period. The runners had only 25% the rate of disability as compared with the control group, and their disability was postponed by 12 years.[45] The data presented by Fries himself in 1980 predicting the course of longevity to date—i.e. a gradual decline in morbidity and mortality in our aging population in association with a precipitous decline in the last year of life—is perhaps the most convincing.[27,38] As a result, per capita Medicare spending has decreased, projected to decline from 6.1% to 4.0% between 2013 and 2022.[39] It has also been found that over the past 20 years Medicare patients in the last year of life consistently consumed a significant 27.4% of Medicare outlays.[31] This figure has been stable for the last several decades within a range of 26.9-30.6%, with 70% of this final amount actually spent in the last 6 months of life.[31]
The prediction that Americans will become more infirm as they age and will therefore utilize more medical care increasing health care costs has been proven wrong. Just recently, the Congressional Budget Office (CBO) also found that total and per capita Medicare spending has grown more slowly than predicted each year from 2010 to 2014. As a result, Medicare spending in 2014 will be about $1200 lower per person than was expected in 2010. The total outlay for 2014 Medicare spending was therefore reduced by $9 billion, from $612 billion to $603 billion.[39] Future Medicare spending is expected to grow at a slower rate than had been projected, remaining constant at about 14% of the federal budget. Thus, as we have seen, both controlled scientific studies and the most recent Medicare data corroborate and lend further confirmation to the validity and reality of the hypothesis of compression of morbidity.
Controlled studies and accurate data on health care costs then are fundamental parameters for studying compression of morbidity—but not so government statistics on disability claims. Thus, we should issue a word of caution as to the possible use of younger-age group disability figures and spurious sociological data, and commingling them with genuine morbidity data in this setting. Both Drs. Emanuel and Fries mentioned “disability” in the broad sense of progressive impairment due to age or chronic illness. But figures in government and sociological literature for legal “disability” associated with financial benefit may inflate genuine morbidity statistics causing spurious “expansion of morbidity.” Many studies suggest that a significant percentage of applicants seeking workers compensation, litigation, and/or receiving “disability” are motivated by secondary or tertiary gain (as such many of these beneficiaries are true malingerers fraudulently abusing the system).[16,17,28,37,40] This is a growing societal problem that seems to be engendered by the collectivist (socialistic) welfare system afflicting much of the West, particularly the United States. Clouded by such sociological and political smoke screens, compression of morbidity may actually be more dramatic than we suppose.
Let us make one more objection before concluding: Emanuel’s epithet of “the American Immortal” is highly misleading—and wrong. Fries never said or even implied that the maximum lifespan is increasing or that compression of morbidity suggests anything approaching immortality. In fact, he admits maximum lifespan presently seems to be fixed, noting that the case of longest documented longevity was 114 years in a person in Japan. Fries arrived at an “ideal” average lifespan of 85 because morbidity, disability, and senescence seem to generally accumulate after that age. Nevertheless, Fries does not deny the possibility that medical progress may in the future push the maximum lifespan further by achieving an increase in the doubling time of human cells and/or an increase in human organ reserve.[27] Presently, it should be noted that the average American (Caucasian) born in 2010 has a life expectancy of 79 years; women 81 years. Longevity of African-Americans has increased in tandem, but reaching a lower life expectancy of 74.5 years. Life expectancy in the U.S. has increased as follows: It was 47 years in 1900; 60 years in 1930; 70 years in 1960; 75 years in 1990. As of 2009, life expectancy reached almost 79 years overall; 76 years for males, 81 for females.[24,38] It is a pity that the secular state has become such a formidable leviathan—a powerful leviathan veritably worshipped as a civil religion by statist politicians as well as private individuals in positions of authority—that they have in rituals of political expediency militated toward sacrificing the age-old dream of healthy longevity on the altar of government rationing.[2,15,19-21]
Conclusion
When I began this project, I was skeptical of Dr Fries’s celebrated compression of morbidity hypothesis. I have now become convinced the hypothesis should be upgraded to theory by the scientific method. It is because of this theory that the aging process can presently be seen in the proper perspective, and affirm that as individuals we can do much to stay “young” and remain vibrant and healthy as we age. Toward this end, we need to pay more attention to the 10 points enumerated earlier on leading healthier lifestyles. When Emanuel asks rhetorically in his article, “Is 70 the new 50?” Many of us who have been fortunate to have known our parents and grandparents can probably answer the question categorically in the affirmative. I believe that today with the prolongation in life expectancy and affirmation of the compression of morbidity theory, as has been outlined, age 60 is indeed the new age 40; 70 is the new 50; and 80 is the new 60 [Figure 10]. I assert life expectancy data and compression of morbidity reflect this current 20 year blessing! Unfortunately, this blessing does not go on forever, and as we reach age 90, the life clock catches up with us and age 90 is therefore not the new 70; morbidity accumulates after the ideal lifespan of age 85. The maximum lifespan holds at age 115.[24] I do not see anything on the horizon or in the futurists’ visions to alter this fact for the time being. There is still hope, though, for an active life until the end of existence for many of us. Fries himself lives by his word; not only has he and his wife Sarah celebrated 50 years together [Figure 11], but he remains active, “having run at least 500 miles each year since 1970,” so writes an admiring colleague. “He has also completed the Boston Marathon and is a high-altitude climber who has reached the peak of the tallest summit on six of the seven continents.” [43]
We don’t need to wait for old age to start. I have already mentioned how Dr. Ausman and Dr. Maroon remain active. Dr. Blaylock pursues his research in nutrition and theoretical neurosciences. As for me, my wife Helen and I exercise daily for one hour as noted, and I hunt deer and razorback feral hogs. We grow vegetables, tend fruit trees for our own vintage wines (i.e. plum, peach, apple, and pear), and generally cultivate our small physical domain but broad intellectual garden. For others, old age is a life of graceful contemplation and intellectual pursuits. In responding to Emanuel’s call for limiting life to age 75 as life not worth living after that, I have made the following reply elsewhere:
I am curious as well as perplexed. Has Dr. Emanuel ever had the interest or time to read Thucydides and Herodotus? I wonder if he ever read Plutarch, Livy, Virgil, or any of the poems of Sappho or Elizabeth Barrett Browning? I wonder if he ever read Plato, Aristotle, or understands the meaning of the Aristotelian good life [Figure 12], and the time and activities that are necessary for the attainment of real happiness and wisdom? The ultimate good life is not necessarily found in our hard-working, intensive, utilitarian, and productive years, but in our years of leisure and contemplation that in today’s stressful and fast-moving society can be attained only in our advancing years. One can also spend those years continuing to fulfill the duties of citizenship, improving one’s community, insisting on better government—e.g. preserving and increasing liberty—for one’s children and grandchildren, hoping they live in a better world.[20]
And so, we must conclude that much can be accomplished in the twilight of our lives; but to preserve health and vitality, we must remain healthy in body and soul, as with Voltaire’s counsel: Cultivating our physical and spiritual garden until the very moment of our death!
Read the Prelude to this article.
Acknowledgment
The author wishes to thank Dr. James I. Ausman for reading the manuscript and making suggestions resulting in the widening of the scope and the betterment of this Review Article. Any errors or omissions, though, are solely my own. The author has no conflict of interest and declares hereby that the project was a labor of love and completely self-funded.
References
1. Aristotle. Nicomachean Ethics (Book X) In: On Man in the Universe. Roslyn, NY: Walter J. Black; 1943. p. 224‑42.
2. Arnett JC. The bioethics movement: An emerging culture of death. Med Sentinel 2002;7:48‑9, 57. Available from: http://www.haciendapub.com/medicalsentinel/bioethics‑movement‑emerging‑culture‑death. [Last accessed on 2011 Jun 08].
3. Ausman JI. Have you made a strategic plan for the rest of your life? CNSQ — Congress Neurol Surg Q 2014;15:12‑3.
4. Baycrest Centre for Geriatric Care. Bilingualism delays onset of Alzheimer’s symptoms, study finds. ScienceDaily. Available from: [Last accessed on 2010 Nov 08].
5. Baycrest Centre for Geriatric Care. Bilingualism has protective effect in delaying onset of dementia by four years, Canadian study shows. ScienceDaily. Available from: [Last accessed on 2007 Jan 12].
6. Blaylock RL. Excitotoxins: The Taste That Kills. Albuquerque, NM: Health Press; 1994.
7. Blaylock RL. Food additive excitotoxins and degenerative brain disorders. Med Sentinel 1999;4:212‑5. Available from: http://www.haciendapub.com/medicalsentinel/food‑additive‑excitotoxins‑and‑degenerative‑brain‑disorders.
8. Blaylock RL. Health and Nutrition Secrets that Can Save Your Life. Albuquerque, NM: Health Press; 2002. p. 232‑4; 272‑3.
9. Blaylock RL. Health and Nutrition Secrets that Can Save Your Life. Albuquerque, NM: Health Press; 2002. p. 215‑350.
10. Blaylock RL. Health and Nutrition Secrets that Can Save Your Life. Albuquerque, NM: Health Press; 2002. p. 270‑1.
11. Blaylock RL. Immunology primer for neurosurgeons and neurologists part 2: Innate brain immunity. Surg Neurol Int 2013;4:118.
12. Blaylock RL. Your golden years: Be healthy, not frail. Blaylock Wellness Rep 2010;7:1‑3.
13. Blaylock RL, Maroon J. Immunoexcitotoxicity as a central mechanism in chronic traumatic encephalopathy‑A unifying hypothesis. Surg Neurol Int 2011;2:107.
14. Blaylock RL, Maroon J. Natural plant products and extracts that reduce immunoexcitotoxicity‑associated neurodegeneration and promote repair within the central nervous system. Surg Neurol Int 2012;3:19.
15. Callahan D. Setting Limits: Medical Goals in an Aging Society. New York: Simon and Schuster; 1988.
16. Carone DA. Physicians should be concerned about malingering. KevinMD.com. Available from: http://www.kevinmd.com/blog/2012/01/physicians‑concerned‑malingering.html [Last accessed on 2012 Jan 15].
17. Carone DA, Iverson GL, Bush SS. A model to approaching and providing feedback to patients regarding invalid test performance in clinical neuropsychological evaluations. Clin Neuropsychol 2010;24:759‑78.
18. Donnelly L. NHS ‘defies the law’ to deny pensioners vital operations, warns Royal College of Surgeons. The Telegraph. Available from: /health/healthnews/ 10942295/NHS‑defies‑the‑law‑to‑deny‑pensionersvital‑operations‑warns‑Royal‑College‑of‑Surgeons.
html [Last accessed on 2014 July 03].
19. Emanuel EJ. Why I hope to die at 75: An argument that society and families — and you — will be better off if nature takes its course swiftly and promptly. The Atlantic. Available from: http://www.theatlantic.com/features/archive/2014/09/why‑i‑hope‑to‑die‑at‑75/379329/[Last accessed on 2014 Sep 17].
20. Faria MA. Bioethics and why I hope to live beyond age 75 attaining wisdom!: A rebuttal to Dr. Ezekiel Emanuel’s 75 age limit. Surg Neurol Int 2015;6:35. Available from:
21. Faria MA. Bioethics — The life and death issue. HaciendaPublishing.com. Available from: . [Last accessed on 2012 Oct 24].
22. Faria MA. Medical history — Hygiene and sanitation. Med Sentinel 2002;7:122‑3. Available from: http://www.haciendapub.com/medicalsentinel/medical‑history‑hygiene‑and‑sanitation
23. Faria MA. Epidemic diseases and public health In: Medical Warrior — Fighting Corporate Socialized Medicine. Macon, GA: Hacienda Publishing, Inc.; 1997. p. 126‑31. Available from: [Last accessed on 2012 Nov 05].
24. Faria MA. In search of the fountain of youth In: Medical Warrior — Fighting Corporate Socialized Medicine. Macon, GA: Hacienda Publishing, Inc.; 1997. p. 121‑5. Available from: http://www.haciendapub.com/articles/search‑fountain‑youth [Last accessed on 2012 Nov 05].
25. Faria MA. Vandals at the Gates of Medicine — Historic Perspectives on the Battle Over Health Care Reform. Macon, GA: Hacienda Publishing, Inc.; 1994. p. 355‑6.
26. Frenda SJ, Patihis L, Loftus EF, Lewis HC, Fenn KM. Sleep deprivation and false memories. Psychol Sci 2014;25:1674‑81.
27. Fries JF. Aging, natural death, and the compression of morbidity. N Engl J Med 1980;303:1305.
28. Gallegos A. Detecting deception: How to handle a malingering patient. American Medical News. Available from: http://www.amednews.com/article/20120910/profession/309109942/4/[Last accessed on 2014 Sep 10].
29. George A. The Epic of Gilgamesh — A New Translation. New York, NY: Barnes and Noble Books; 1999.
30. Henrichs I, Froesch D, Wolf AS, Teller WM. Impact of apolipoprotein E on Alzheimer’s disease. Curr Alzheimers Res 2013;10:809‑17.
31. Hogan C, Lunney J, Gabel J, Lynn J. Medicare beneficiaries’ cost of care in the last year of life. Health Aff 2001;20:188‑95.
32. Huang EJ, Reichardt LF. Neurotrophins: Roles in neuronal development and function. Annu Rev Neuroscie 2001;24:677‑736.
33. Jacobs E. Longevity is here to stay — embrace it. Financial Times. Available from: http://www.ft.com/cms/s/0/30419b9c‑bf2a‑11e3‑a4af‑00144feabdc0.html [Last accessed on 2014 Apr 09].
34. Kralovics R, Passamonti F, Buser AS, Teo SS, Tiedt R, Passweg JR, et al. A gain‑of‑function mutation of JAK2 in myeloproliferative disorders. N Engl J Med 2005;352:1779‑90.
35. Maroon JC. The evolution of life and career. CNSQ — Congress Neurol Surg Q 2014;15:16‑7.
36. Maroon JC. The Longevity Factor: How Resveratrol and Red Wine Activate Genes for a Longer and Healthier Life. New York: Simon and Schuster; 2009.
37. Mittenberg W, Patton C, Canyock EM, Condit DC. Base rates of malingering and symptom exaggeration. J Clin Exp Neuropsychol 2002;24:1094‑102.
38. National Vital Statistics Report. Centers for Disease Control and Prevention. United States Life Tables. 2014;62:1‑63. Available from: [Last accessed on 2009 Jan 06].
39. Neuman T, Cubanski J. The mystery of the missing $1,200 per person: Can Medicare’s spending slowdown continue? Kaiser Family Foundation. Available from: http://kff.org/health‑costs/perspective/the‑mystery‑of‑the‑missing‑1000 ‑per‑person‑can‑medicares‑spending‑slowdown‑ continue/[Last accessed on 2014 Sep 29].
40. Pawl R. When the pain won’t wane it’s mainly in the brain. Surg Neurol Int 2013;4(Suppl 5):330‑3.
41. Russell J. Delaying Parkinson’s disease. Today’s Geriatric Medicine September/October 2009;2:24. Available from: [Last accessed on 2009 Oct 05].
42. Sadigh‑Eteghad S, Talebi M, Farhoudi M. Association of apolipoprotein E epsilon 4 allele with sporadic late onset Alzheimer’s disease, a meta‑analysis. Neurosciences (Riyadh) 2012;17:321‑6.
43. Swartz A. James Fries: Healthy aging pioneer. Am J Public Health 2008;98:1163‑6.
44. Vita AJ, Terry RB, Hubert HB, Fries JF. Aging, health risks, and cumulative disability. N Engl J Med 1998;338:1035‑41.
45. Wang BW, Ramey DR, Schettler J D, Hubert HB, Fries JF. Postponed development of disability in elderly runners: A 13‑year longitudinal study. Arch Intern Med 2002;162:2285‑94.
46. Weinberg L, Hasni A, Shinohara M, Duarte A. A single bout of resistance exercise can enhance episodic memory performance. Acta Psychol 2014;153:13‑9.
47. Yamada K, Nabeshima T. Brain‑derived neurotrophic factor/TrkB signaling in memory processes. J Pharmacol Sci 2003;91:267‑70.
Article written by: Dr. Miguel Faria
Miguel A. Faria, Jr., M.D. is Clinical Professor of Surgery (Neurosurgery, ret.) and Adjunct Professor of Medical History (ret.) Mercer University School of Medicine. He is an Associate Editor in Chief and a World Affairs Editor of Surgical Neurology International (SNI), and an Ex-member of the Injury Research Grant Review Committee of the Centers for Disease Control and Prevention (CDC). 2002-05; Former Editor-in-Chief of the Medical Sentinel (1996-2002), Editor Emeritus, the Association of American Physicians and Surgeons (AAPS); Author, Vandals at the Gates of Medicine (1995); Medical Warrior: Fighting Corporate Socialized Medicine (1997); and Cuba in Revolution: Escape From a Lost Paradise (2002).
This article was originally published in Surg Neurol Int 2015;6:49. This article can be cited as: Faria MA. Longevity and compression of morbidity from a neuroscience perspective: Do we have a duty to die by a certain age? Surg Neurol Int 2015;6:49. Available from: https://surgicalneurologyint.com/surgicalint-articles/longevity-and-compression-of-morbidity-from-a-neuroscience-perspective-do-we-have-a-duty-to-die-by-a-certain-age/
Copyright ©2015-2019 Miguel A. Faria, Jr., MD