- Articles
Book Review: The Frontal Lobes and Neuropsychiatric Illness. Reviewed by Miguel A. Faria, MD
The Frontal Lobes and Neuropsychiatric Illness (2001) by Drs Stephen P. Salloway, Paul F. Malloy, and James D. Duffy (editors) provides an excellent summation on the state of knowledge of prefrontal lobe dysfunction in neuropsychiatry. It is written in four parts. Part 1 is Introduction; Part 2, “Functional Organization of Prefrontal Lobe Systems” consists of 5 chapters; Part 3, “Prefrontal Syndromes in Clinical Practice” consists of 4 chapters; and Part 4, “Frontal Lobe Dysfunction in Neuropsychiatric Disorders” is composed of 5 chapters — 16 chapters and 264 pages in all. The book is fully illustrated and pages are of ample size, ideal for graphs, tables, photographs, and other illustrations. The book is well organized and the chapters vary in the quality of the presentation and depth, depending on the experts who wrote them. The majority of the 26 writers are psychiatrists, followed by neurologists and other neuroscience specialists. There are only three neurosurgeons, and only the final chapter is written from the perspective of neurosurgery. This is a bit of a shame because neurosurgeons are the researchers and clinicians who have in vivo access to the frontal lobes of surgical patients, and they could have brought a more clinical and surgical perspective into this tome, which at times is heavy on abstract research and various theoretical models. I will come back to this later.
With that said, several of the authors make a good case and expound that the frontal lobe syndrome — in addition to the well-known focal deficits involving the Primary Motor Cortex and the Frontal Eye Fields — consists of three other major neuropsychiatric syndromes. These three clinical subtypes are frequently seen in clinical practice intermixed with one another — once again making the conventional term Frontal Lobe Syndrome still very useful and irreplaceable for clinicians, particularly neurologists and neurosurgeons, perhaps even for psychiatrists.
Frontal lobe dysfunction can be categorized according to the prevailing clinical subtypes. These three subtypes reflect disruption of the neural circuit underlying the prefrontal lobe cortical connections to subcortical structures. These circuits function together in anatomic, physiologic and biochemical basis in preserving frontal lobe function. Generally, these circuits run from cortical areas of the prefrontal regions to the basal ganglia (striatum), from caudate nucleus to globus pallidus to dorsomedial nucleus of the thalamus, and back to cortex. This is an example of a primary direct loop, but there are other indirect loops that may feed into the system.
Chapter 3 contains magnificent photographs, including one coronal cut of the brain with direct and indirect frontal subcortical loops, indicating neurotransmitter excitatory and inhibitory connections, among these structures in the circuitry (page 17).
Frontal lobe impairment in neuropsychiatric syndromes involves one of three clinical subtypes, depending on the involvement of the specific prefrontal area and its subcortical connections.
The first syndrome involves damage to the Dorsolateral Prefrontal area, which is responsible for the executive action of the brain. Disruption of this circuit, either in the cortex or deeper structures, results in the dysexecutive or the disorganized syndrome. This subtype includes deficits in organizational activity (as in executive functions), diminished judgment, poor cognition and learning, poor memory recall, concrete interpretation of abstract concepts, poor word fluency, perseveration, verbal-manual dissociation, and I suspect that if elicited on neurological examination, there would be positive frontal release signs, such as grasp and snout reflexes.
The second syndrome relates to lesions in the Orbitofrontal area, which consists of medial and lateral orbitofrontal cortices. Deficits in these areas and related subcortical connections result in personality changes, such as anergy, irritability, tactlessness, impulsivity and distractibility, a constellation of symptoms epitomized by loss of social restraints. In clinical practice we have used the term disinhibition and have frequently observed an accentuation of unfavorable or disadvantageous personality traits. For example, withdrawn personalities become apathetic, and aggressive ones, belligerent. With damage confined to the medial aspect of the orbitofrontal cortex, neuro-vegetative changes are seen, such as hypo or hyperphagia, in addition to the aforementioned constellation of symptoms. Most interesting, the authors have also linked obsessive compulsive disorders to both medial and lateral damage of the orbitofrontal cortex. Labile affect and mania, as well as utilization behavior, were also noted more frequently with lateral orbitofrontal dysfunction.
The third syndrome is caused by lesions of the Anterior Cingulate area, which consists of the prefrontal area in the anterior cingulate gyrus and the supplementary motor area. Lesions to this complex circuit result in diminished spontaneity, poverty of speech, apathy, urinary incontinence without affectation, diminished verbal (mutism) to motor (akinesia) behavior.
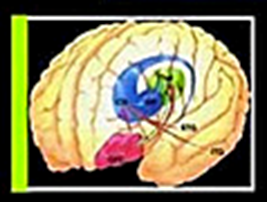
Chapter 4 is also a magnificent chapter loaded with information and many illustrative figures. I found the color drawings on pages 47 and 48 outstanding and essential for understanding the lateral and medial orbitofrontal cortices (OFC) and their associated basal ganglia (BG) loops. To reinforce these connections, the figure on page 47 shows the lateral orbitofrontal cortex (OFC) and the superior temporal (STG) and inferior temporal (ITG) gyri sending output to the caudate nucleus (CN) that in turn relays inhibition to the globus pallidus (GP), that in turn inhibits the thalamus (Thal), which in turn excites the cortex closing the loop. In figure 48, the orbitofrontal cortex (OFC) sends impulses to the ventral striatum (VS) and has reciprocal connections to the thalamus. But here we also have the entorhinal (ENT) cortex, STG, ITG, anterior cingulate area (ACA) and amygdala (AMG) to the VS which in turn inhibits the GP that also sends inhibitory output to the thalamus. The latter closes the loop sending excitatory connections to the medial OFC and the related cortical regions of the temporal lobe. Among the subcortical structures only the thalamus and the subthalamic nucleus are shown to send excitatory glutaminergic fibers to the GP and subtantia nigra via an indirect loop. In reference to these limbic and subcortical connections, the editors have also published another seminal work in neuropsychiatry, .
Chapter 5 will be discussed later in conjunction with schizophrenia. Chapters 6 and 7 propose new theoretical models to study frontal lobe function that would replace conventional terminology and traditional thinking paradigms. In fact not only in these chapters, but also in more clinical ones, many statements are made to the effect of advocating the use of new terms and need for the formulation of new theoretical models that supposedly make old terms and traditional clinical verbiage obsolete. For example, several writers proposed the abandonment of the term frontal lobe syndrome; another condescendingly referred to “so-called ‘release signs,’ ” etc. Some of the researchers instead advocate for the use of their own terminology and theoretical models, which I for one found clumsier, at times unworkable, because these new paradigms have been gathered from non-human primates and other laboratory animal research, and their functional anatomy cannot always be extrapolated to the human brain. For example, Chapter 6 promises to introduce a “distinct approach to hemispheric specialization called novelty-routinization continuum…” because the authors assert that “traditional assumptions” about the lateralization of language to the left hemisphere and the processing of information in the right hemisphere “are not so clear cut.” Reading these chapters and some sections in other chapters, I found myself more confused when I finished that when I started. The new terminology and concepts proposed were more complex than advertised and certainly less useful — more likely to complicate and obfuscate rather than simplify and clarify. I think clinicians will stick to the “traditional assumptions,” such as conventional laterality, as to the left hemisphere being largely responsible for linguistics and the right hemisphere for information processing — despite the alleged shortcomings of these generalizations — until better, more workable models fitting the clinical picture come along for better understanding of patients’ clinical illnesses and for better verbal communication with their families.
In contradistinction to the theoretical chapters with novelty paradigms, Chapters 9 through 16 are more clinical and practical. In those chapters I found that many new terms and research findings were very useful, and that new paradigms could be incorporated within clinical practice by working neurologists and neurosurgeons at the bedside.
An outstanding section in Chapter 9 lists both neuropsychological tests as well as clinical signs that can be elicited at the bedside in the differentiation of the five frontal lobe subsystem’s damage. This chapter also provides corroborative evidence that the three subtypes of prefrontal lobe dysfunction arise from lesions of the frontal lobe-striatal-thalamic circuit and are frequently mixed, although as mentioned previously one subtype may predominate.
Chapter 10 provides a nice clinical summary of neuropsychiatric disorders with nine illustrative cases. It also provides a pharmacological basis for these disorders, citing the specific neurotransmitters associated with them, and thus the postulated benefit of the manipulation of psychotropic drugs that may be used to treat these neuropsychiatric illnesses.
Chapter 12 discusses frontal lobe dysfunction in secondary depression and reveals the intriguing finding that on fluorodeoxyglucose positron-emission tomography (PET) studies bilateral inferior frontal lobe hypometabolism is seen in patients with secondary depression regardless of the underlying pathology. Patients with Parkinson’s disease, Huntington’s disease, and stroke cases had this similar finding; whereas the studies on these neurologically-afflicted patients were normal when they were not depressed. The same findings of hypometabolism were found in the temporal lobes of depressed patients; whereas normal temporal lobe metabolism was noted in non-depressed patients. Of further interest is that the temporal lobes were more sensitive to mood changes in that manic patients showed temporal lobe hypometabolism ipsilateral to the lesion, whereas depressed patients, as we have seen, had bilateral findings. Moreover, patients with deep striatal strokes with motor symptoms had entire ipsilateral hemisphere hypometabolism, whereas patients with non-motor strokes had a restricted abnormality in the ipsilateral prefrontal lobe cortex only.
Schizophrenia, a disease that has been implicated in frontal lobe disease, was not neglected in this book. One of the authors (Chapter 5) implicated a defect in working memory as the possible impairment in this devastating mental illness. Working memory is the term used to denote transient memory that is used for short periods of time in information processing allowing continuity between incoming information (or environmental stimulus) and the proper response to that information. The frontal lobes use working memory to respond to different contingencies, such as responding to developing situations in accordance with stored information rather than reflexive reactions to immediate stimulation. Lacking working memory, as postulated for schizophrenia, would cause disconnection of information and processing, and a lack of an appropriate response — “out of sight, out of mind.” This hypothesis could help explain the thought disorder underlying schizophrenia and frontal lobe findings, as further elaborated in Chapter 13. Lack of attention, lack of initiative, disrupted cognition, confusion, and the myriad other defects commonly seen in schizophrenia may represent a disconnection between the dorsolateral prefrontal cortex and the temporoparietal association areas and the underlying limbic structures, not to mention a disruption of the summation of excitatory and inhibitory signals received from the various neurotransmitters utilized in the cortical and subcortical circuits. Although the clinical diagnosis of schizophrenia is easily made at the bedside, the underlying neuropathology and/or biochemical basis for the clinical picture are yet to be fully elucidated.
Perhaps the most fascinating sections are in Chapter 15, “The Frontal Lobes and Content-Specific Delusions.” Here we learn of the underlying psychopathology of content-specific delusions (CSD) — i.e., delusions that have a single theme, such as in the reduplicative paramnesias where a place is duplicated. In Capgras syndrome, a reduplicative delusion of person, the patient believes a family member is an impostor. A good example of this is seen in the old and new versions of the film The Invasion of the Body Snatchers, except that the impostors in the movie are real duplications by aliens! In the Doppleganger syndrome, a subjective double delusion, the patient believes he has a double. The Othello syndrome or delusional jealousy is a sexual delusion in which the patients are convinced their spouses are having amorous affairs with other persons. The Clérambault syndrome is another sexual delusion (erotomania) in which the patients believe that they are having an affair, usually with famous persons. Here, the film Taxi Driver comes to mind, and the actualization was attempted with John Hinckley trying to assassinate President Ronald Reagan to secure the heart of actress Jodie Foster.
Numerous other delusions are discussed and the underlying psychopathology explained. Most surprising is that many of these delusions have an underlying pathological basis, from brain tumors, to strokes, degenerative diseases, and metabolic disorders. But sadly, the researchers found that many of the medical records did not even contain neurological examinations, much less CT scans or EEGs, so the findings were incomplete. It was on those relatively few cases that had full medical work-ups that structural lesions were found. In those cases, a finding was very intriguing, and that was, that these CSD patients usually had right hemisphere or bilateral frontal lesions confirmed by neuroimaging studies, EEG, or at autopsy.
What I have written in this book review is a very brief survey of selective features contained in this excellent book that turns out to be a cornucopia of valuable information on the role of the frontal lobes in neuropsychiatry. Despite my mild criticisms of several chapters, overall this tome is strongly recommended to students, as well as clinicians. Researchers in this fascinating field of neuropsychiatry will also find this tome a useful reference source and a possible springboard for further research on these areas of the brain, previously referred to as silent, sort of terra incognita, now opened by researchers to further exploration.
Reviewed by Dr. Miguel Faria
Miguel A. Faria, M.D., is Associate Editor in Chief in socioeconomics, politics, medicine, and world affairs of Surgical Neurology International (SNI). He was appointed and served at the behest of President George W. Bush as member of the Injury Research Grant Review Committee of the Centers for Disease Control and Prevention (CDC), 2002-2005. He is the author of Vandals at the Gates of Medicine (1994). His recently released book is America, Guns, and Freedom: A Journey Into Politics and the Public Health & Gun Control Movements (2019).
The Frontal Lobes and Neuropsychiatric Illness by Dr Stephen P. Salloway, Dr Paul F. Malloy, and Dr James D. Duffy, editors. ISBN-13: 978-0880488006; ISBN-10: 088048800X. Washington, DC; American Psychiatric Publishing, Inc.; 1st Edition (May 1, 2001).
This article may be cited as: Faria MA. Book Review of The Frontal Lobes and Neuropsychiatric Illness. HaciendaPublishing.com, December 28, 2020. Available from: https://haciendapublishing.com/book-review-the-frontal-lobes-and-neuropsychiatric-illness-reviewed-by-miguel-a-faria-md/(opens in a new tab)
The version of this article that was also published in Surgical Neurology International may be cited as: Faria MA. Frontal lobe syndromes in neuropsychiatry – A book review. Surg Neurol Int 16-Dec-2020;11:439. Available from: https://surgicalneurologyint.com/surgicalint-articles/frontal-lobe-syndromes-in-neuropsychiatry-a-book-review/
Copyright ©2020 Miguel A. Faria, Jr., M.D.