- Articles
Violence, mental illness, and the brain — A brief history of psychosurgery: Part 3 — From deep brain stimulation to amygdalotomy for violent behavior, seizures, and pathological aggression in humans
Abstract — In the final installment to this three-part, essay-editorial on psychosurgery, we relate the history of deep brain stimulation (DBS) in humans and glimpse the phenomenal body of work conducted by Dr. Jose Delgado at Yale University from the 1950s to the 1970s. The inception of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research (1974-1978) is briefly discussed as it pertains to the “determination of the Secretary of Health, Education and Welfare regarding the recommendations and guidelines on psychosurgery.” The controversial work — namely recording of brain activity, DBS, and amygdalotomy for intractable psychomotor seizures in patients with uncontrolled violence — conducted by Drs. Vernon H. Mark and Frank Ervin is recounted. This final chapter recapitulates advances in neuroscience and neuroradiology in the evaluation of violent individuals and ends with a brief discussion of the problem of uncontrolled rage and “pathologic aggression” in today’s modern society — as violence persists, and in response, we move toward authoritarianism, with less freedom and even less dignity.
DEEP BRAIN STIMULATION (DBS) EXPERIMENTS IN HUMANS
In the mapping of the brain in cerebral localization, neurosurgeon Dr. Wilder Penfield found that neither epilepsy nor electrical stimulation of the brain (ESB) at the surface of the cerebral cortex elicited emotional reactions in humans.[26] Dr. Jose Delgado found this to be mostly true, but there were exceptions. In contrast, ESB via deeply implanted electrodes in localized areas of the brain (DBS) elicited both pleasurable and aversive responses in man.
Pain, rage, and fear have been evoked or calmed by DBS in various structures of the brain, including hypothalamus, thalamus, amygdala, and the ventral tegmental area (VTA) in animals and man. Stimulation of the dorsolateral thalamus has evoked anxiety, fear, and premonitions of disaster in humans, corresponding to the intensity of the DBS. Conversely, anxiety has been relieved by localized lesions of the frontal lobe and thalamus, and lesions in the medial thalamus and the cingulum have relieved chronic cancer pain.[2,14,29]
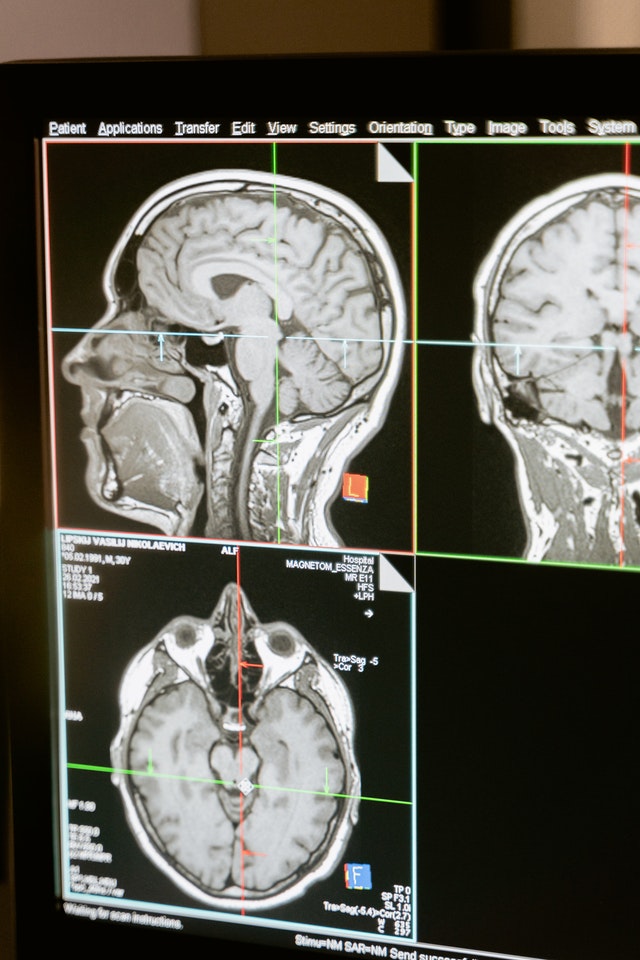
Stimulation of the amygdala produced intense fear or rage, essentially producing electrically induced aggression in humans [Figure 1].[11,20] Nevertheless, normally this induced aggression is modified by moral and social constraints so that the experimenters are not usually attacked. Animals such as rats, cats, and monkeys, Delgado found, learned quickly to stimulate themselves by voluntarily triggering ESB to deep cerebral structures that reward them with pleasurable sensations, while passively or actively avoiding ESB/DBS that elicited aversive punishment or painful stimulation.[15] Their response rate, indicating the strength of the pleasurable sensations in different areas, could be recorded. For example, Delgado recorded rates of pressing of a lever of up to 5000/hour for DBS in the hypothalamus, and 200/hour in the rhinencephalic areas. On the other hand, once the animals had pressed the lever one time triggering a painful stimulus, they ceased pressing that lever or stopped crossing an electric field[4] [See Table 1 below for a summary of experimental responses in animals].
DBS of the septal areas of schizophrenics have resulted in enhanced alertness, cooperation, and pleasurable sensations, even euphoria. Patients with narcolepsy and psychomotor seizures have also reportedly experienced euphoria and sexual thoughts with self-elicited DBS of the septal areas. Activation of these areas with local neural discharges has also been achieved by injection of chemical substances, such as acetylcholine, producing euphoria and “orgastic sensations.” The beneficial results of DBS in major depression have also been documented in a few instances in which patients were provided with portable stimulators for self-treatment.[4,15]
To facilitate his work of ESB, Delgado invented a “stimoceiver,” a radio transmitter and receiver, which was used to remotely stimulate the brain electrically via the usual, deeply implanted electrodes, while via another channel the electroencephalography (EEG) brain waves could be recorded. No longer were his animal or human subjects restrained by wires.[5,21] The test subjects were free to move around while the experimenter could stimulate, observe, and record the behavioral and electronic responses. Delgado also invented a “chemitrode,” an implantable device that could be used to inject and slowly release chemical substances into test subjects, a forerunner of the implantable reservoirs and catheters used by neurosurgeons today.
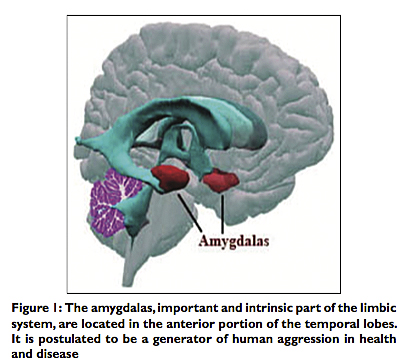
In Chapter 14 of his magnum opus, Physical Control of the Mind (1986), Delgado wrote: “Ours is a tragically unbalanced industrial society which devotes most of its resources to the acquisition of destructive power and invests insignificant effort in the search which could provide the true weapons of self-defense: Knowledge of the mechanisms responsible for violent behavior.”[4] In the study of violent behavior and unprovoked aggression in which psychopathic individuals use naked force with the intent of hurting others, Delgado lamented, “Attention is directed to economic, ideological, social, and political factors and to their consequences, which are expressed as individual and mass behavior, while the essential link in the central nervous system (CNS) is often forgotten”[4] [Figure 2]. In other words, both intrinsic neurophysiologic and external environmental factors must be evaluated. This has not been done comprehensively, not only because of cost but also most revealing politically, because of the zeitgeist of the times since the 1970s. Most of Delgado’s achievements have been ignored, judged if at all superficially as “inconclusive,” if not virtually forgotten – and when occasionally rediscovered, referred to as “mind control experiments” and relegated to the realm of diabolical conspiracy theories or science fiction.[32]
PSYCHOMOTOR SEIZURES, VIOLENCE, AND THE AMYGDALA IN HEALTH
AND DISEASE
This subheading and the one following are derived to a significant degree from the fascinating and controversial book, Violence and the Brain (1970) by neurosurgeon Vernon H. Mark, MD. and psychiatrist Frank R. Ervin, MD., as well as the work of Dr. Jose Delgado, who collaborated with these authors in the chapters that I am referencing in this section.[21,22]
The limbic system, as we have discussed, evolved from the reptilian brain, also referred to as the primitive “emotional brain,” and its functions range from vegetative autonomic nervous system (ANS) modulations as to maintain homeostasis in a passive, living organism, to active, aggressive responses necessary for survival. American physiologist Walter Cannon M.D. (1871-1945), who coined the term, “fight or flight” in 1916, asserted, “fear, rage, and pain and the pangs of hunger are all primitive experiences which human beings share with the lower animals.”[3] It is also the limbic system or Papez circuit that is responsible for the modulation and control of “fight or flight” reactions essential for survival.[11,20]
Controlled aggression may be necessary for survival, particularly in animals, but uncontrolled rage leading to unprovoked violence is not. In fact, “pathologic aggression” is in many cases the result of abnormal brains in mentally ill individuals, asserted Dr. William H. Sweet (1911-2001), Professor and Chief of Neurosurgery at Harvard (1961-1977), and many of his colleagues, including the aforementioned neuroscientists, Drs. Mark and Ervin.[12,20,29]
In cases of brain psychopathology, social or penal rehabilitation of young criminal offenders – whose brains have passed the critical developmental period in childhood or adolescence – the present techniques of attempting modification of their environment would be ineffective. Instead, after the proper neurologic evaluation and proper diagnosis, these investigators asserted, more effective treatments would be pharmacologic, or as a last resort, functional neurosurgery. Mark and Ervin pointed to experiments in cats that supported their theory. Grown in total darkness, visual pathways do not develop. But up to a certain age, the optic neural connections retain the capacity to develop, and the cats are able to see when light is restored. Pass a certain critical point, the pathways degenerate and die, and vision cannot be restored.
A similar phenomenon can take place with monkeys during maternal–infant bonding. If bonding is not allowed to take place, or if social interaction is not permitted after a critical period, the monkeys grow up to be “incurably deviant monkeys.”[13]
Ethological researchers attempted to define fixed patterns of violent behavior and aggression in animals in the 1940s. But by the 1960s and 1970s they still continued to disagree as to the relative contributions of “nature versus nurture” to aggressive behavior in animals.[19,23] Mark and Ervin believed both contributions occurred at various levels of the CNS, and that these relative contributions were modified by both learning and neural development. Controlled aggression in normal fight or flight reactions is present in man but it is modified by learning and mollified by social and moral controls. In contrast, pathologic aggression and uncontrolled violence may be the result of structural brain damage from congenital or chromosomal disorders or from later trauma to the CNS, encephalitis, tumors, etc., that may affect the temporal lobes (e.g., epilepsy or psychomotor seizures) or other areas of the limbic system and result in abnormal criminal behavior and/or uncontrolled violence.[20]
In Chapter 6, “The Surgery of Violence,” Mark and Ervin quote an aphorism of Hippocrates, “Extreme remedies are very appropriate for extreme diseases.” Then they go on to discuss the evaluation and psychosurgical management of several fascinating cases of “pathologic aggression,” which they found to be associated with temporal lobe seizures, and more specifically, epileptic discharges emanating from the diseased amygdalas of many of these patients. I will describe one of their illustrative cases at length.
“Julia S” was an attractive 21-year-old girl, “a cherubic blond and daughter of a professional man,” but she had a history of psychotic behavior, associated with uncontrolled rage and sudden violent outbursts, and epilepsy in the mid 1960s. She had been afflicted with encephalitis at age 2 complicated by a seizure disorder that developed at age 10. The seizures were of two types: Sometimes they were typical grand mal seizures; more frequently though, she had temporal lobe epilepsy or psychomotor seizures, “consisting most of the time of brief lapses of consciousness, staring, lip smacking and chewing.” Often following these bouts of temporal lobe epilepsy,” she would be overcome by panic and run off as fast as she could without caring for destination. Her behavior between seizures was marked by severe temper tantrums followed by extreme remorse.”[20]
Julia had incurred two suicide attempts, and on two occasions had brutally assaulted innocent bystanders. In one instance, after experiencing one of her “racing spells” (one of Julia’s descriptions for her psychomotor seizures), she suddenly attacked and plunged a knife at a lady at a theater, followed by one of her panic attacks. On another occasion, the victim was attacked at a mental hospital where Julia was undergoing therapy. This time Julia grabbed a pair of scissors and stabbed a nurse in the chest. The nurse survived the penetrating lung injury, and so did the lady at the theater, but there was no question Julia was a danger to herself and others. She had not responded to either psychotherapy or electroconvulsive therapy (ECT).[20]
It is not clear whether Julia was treated with anticonvulsants during this time. Carbamazepine (Tegretol), which later became the treatment of choice for temporal lobe epilepsy, would not become available in the U.S. until 1974. Phenytoin (Dilantin) had been approved by the Food and Drug Administration (FDA) for generalized seizures in 1953 and became widely used after its literary debut in the 1962 novel, One Flew Over the Cuckoo’s Nest, which in 1975 was made into a widely acclaimed movie starring Jack Nicholson and Louise Fletcher. In the 1960s, Drs. Mark and Ervin had also evaluated some patients with seizures and violent behavior, who had been treated with phenytoin with varying degrees of improvement with or without psychosurgery.
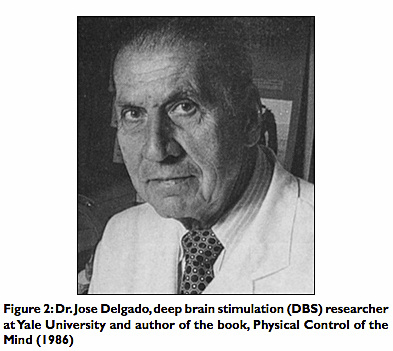
In 1968, as a last resort, Julia was referred to Drs. Mark and Ervin, who as part of her workup performed an EEG that showed epileptic spikes in both temporal lobes. Electrodes were then implanted stereotactically into epileptogenic foci [Figure 3]. Electronic recordings revealed epileptiform activity coming from both amygdalas. DBS of either amygdala induced reproduction of the initial phases of her psychomotor seizures. The left amygdala was chosen for a radiofrequency destructive lesion because it had a more active epileptogenic focus, and an ablative lesion (amygdalotomy) was carried out in this diseased area of the limbic system.[20]
At this point, Dr. Jose Delgado of Yale was consulted, and he brought his new research creation, “the stimoceiver,” whereby they were able to “observe the interactions between the brain stimulations and environmental cues.” Julia was carefully observed, and her brain waves recorded, while under close observation by Drs. Mark, Ervin, and Delgado.[5,21] In the photograph, Julia is seen in a good mood and behavior before stimulation [Figures 4 and 5].
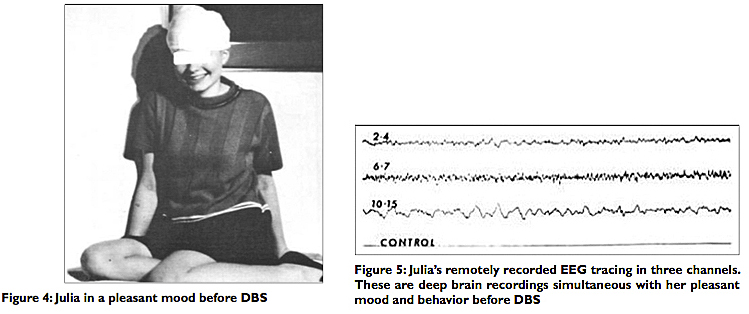
During observation on one of those occasions, simultaneous with a sudden, spontaneous electrical discharge from the right amygdala, Julia ran over to the wall of her bedroom. “Once there, she narrowed her eyes, bared her teeth, and clenched her fists — that is, she exhibited all the signs of being at the verge of making a physical attack.”[20]
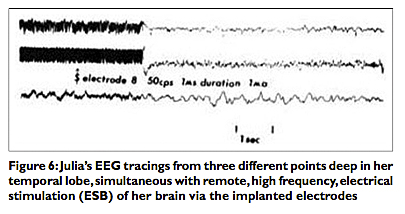
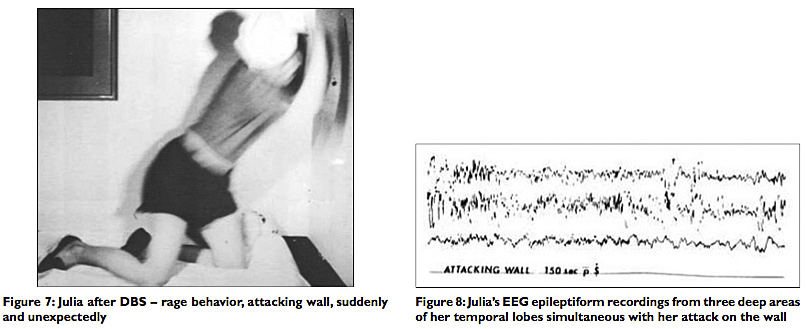
There were three channels of recording on the stimoceiver. The top tracing recorded Julia’s electrical activity in the right anterior amygdala; the second, in the posterior amygdala: The third, behind the amygdala in the hippocampus. Spontaneous electrical discharges stemming from the right amygdala correlated with Julia’s persistent uncontrolled rage behavior. In the illustrated tracings, we can see the results of electrical, radiofrequency DBS of her brain on the EEG tracings [Figure 6]. Electrical stimulation via the deeply implanted electrodes (DBS) evoked an angry mood “with facial grimacing, lip retraction, and signs of threat display” followed by rage attacks, corresponding to the changes in her EEG tracings [Figures 7 and 8].
Her rage, spontaneous or induced by DBS, was reminiscent of what Dr. William H. Sweet later called “pathological aggression”[12,29] [Figure 9].
Because Julia’s violent behavior and psychiatric symptoms persisted, stemming from the opposite amygdala, an ablative lesion was made in the right amygdala. Subsequently, there was some behavioral improvement but the epileptic disorder persisted and her psychotic episodes continued. After 2 years, she had improved with no more rage attacks despite “impulsive anger.” Her psychosis continued “but she was able to live at home, sing in the choir, attend daily adult education classes, and pass her high school equivalency examinations.”[22]
FUNCTIONAL NEUROSURGERY AND THE TERMINAL MAN
When I was a premedical student at the University of South Carolina (USC) in Columbia, my minor was psychology. I wanted to go on and enroll in medical school and specialize in neurosurgery, but I still had a hidden attraction to psychiatry. Indeed, Physiological Psychology and Abnormal Psychology in the summer of 1972 and the spring of 1973 were two of my most fascinating courses. It was then I learned about Professor Jose Delgado, M.D., Ph.D. (1915-2011) at Yale University and his incredible and prolific work with stimulation of deep structures in the brains of animals and humans via implanted microelectrodes. I learned about DBS of the “pleasure centers” of laboratory rats, and how these rodents would learn to stimulate themselves, literally to death, by breaking in and out of an electric field. By crossing back and forth, the rats triggered an electric shock in the deeply implanted electrodes that stimulated their “pleasure centers” located in the septal area of their brains. These rats refused to eat, drink, or mate, for the sake of triggering endless stimulation, and they gradually learned to do this by just simply turning their heads to break in and out of the electric field! I also learned about lesions in the ventromedial nucleus of cats producing rage reactions and fat tomcats, whereas lateral hypothalamic lesions produced docile, scrawny, pathetic kittens, so graphically depicted in the wonderful works of medical illustrator, Dr. Frank H. Netter (1906-1991) in The Ciba Collection of Medical Illustrations.
I also learned about the work of Harvard Medical School neurosurgeon, Dr. Vernon H. Mark, Director of Neurosurgery at Boston City Hospital, and his accomplished associate, Professor of Psychiatry Dr Frank R. Ervin, in the 1960s [Figure 10]. Based on the work and techniques developed by Delgado, Mark and Ervin carried out research on electroencephalographic recordings on the skull (EEG), cerebral surface, as well as deep structures of the brain, as we discussed in the preceding section. [See Table 2 below for a summary of clinical and experimental responses to DBS and ablative lesions in humans] They studied patients with uncontrolled aggression and found that many of them had abnormalities of the brain causing their temporal lobe epilepsy or psychomotor seizures. We have discussed at length the poignant case of Julia S.
These two men collaborating closely postulated (and frequently found) that electroencephalographic (EEG) and structural abnormalities in the diseased temporal lobes were caused by congenital anomalies, such as hamartomas and chromosomal abnormalities; neoplasm such as gliomas; and infections resulting in diffuse encephalitis. Nevertheless, most often the culprit was trauma to the anterior poles and base of the temporal lobes, causing mesial sclerosis, dilated temporal horns, and scarring with epileptogenic foci detectable by surface or deep brain electrode recordings. They believed many patients with temporal lobe abnormalities, particularly those deep in the amydalas, developed psychomotor seizures that were often responsible for their violent behavior, episodes of rage, uncontrolled aggression, and criminal records.[12,20]
Many of these patients went undiagnosed and ended up sometimes in mental institutions but more often they roamed the streets perpetrating crimes until arrested and ending in prison. Psychiatrists (and occasionally neurologists) evaluated these patients — and because many of them did not improve with either psychotherapy or anticonvulsant drugs, remaining dangerous to themselves or others — they were referred to Drs. Mark and Ervin as a last resort. If electrode recordings revealed surface or deep brain epileptiform activity corresponding to their psychomotor seizures and abnormal violent behavior, they were treated by deep brain electrical stimulation or amygdalotomy. For 20 years, Mark and Ervin evaluated and treated these selected patients with uncontrolled violence and incapacitating temporal lobe epilepsy. Approximately 20 amygdalotomies were performed, with many patients improved but not necessarily cured. Their work was described and published in the aforementioned controversial book, Violence and the Brain (1970). Unlike psychologist B. F. Skinner, who promulgated that society had gone beyond the old concepts of freedom and individual dignity in the pursuit of progress, and whose book was a sensation — Mark and Ervin were pilloried for their concept of violence associated with neurosurgically treatable brain disease.[12,20,28,30]
One of the patients whom the Harvard professors treated was to bring them unwelcomed notoriety and embroiled them in controversy. And to add sensationalism to the affair, just about the time that the patient, Mr. Leonard A. Kille, was under their care (1968-1969), a young Michael Crichton (1942-2008), who later became a famous and best-selling author of medical fiction and thrillers, was doing a clinical rotation under Dr. Ervin at Boston City Hospital [Figure 11]. After completing his rotations and obtaining his medical degree from Harvard in 1969, Dr. Crichton too was dragged into the controversy. In fact, the lawsuit controversy stemmed in part from the publication of Crichton’s medical thriller, The Terminal Man, in 1972. The patient and his family alleged that “Thomas R,” the clinical case of the engineer described in Violence and the Brain, was based on Mr. Kille’s case. Moreover, the patient alleged that he was worsened under the doctors’ surgical treatment, and that his case was also the subject of Michael Crichton’s thriller, without his consent.[30] Crichton’s book was adapted into a movie, starring George Segal and Joan Hackett, and was released in 1974.
In the novel, The Terminal Man, Harry Benson suffers from severe blackouts due to psychomotor epilepsy. During these attacks, Benson behaves abnormally and is prone to violence, but remembers nothing afterwards. Deep brain electrodes are implanted, and Benson learns to trigger the seizures because they are pleasurable. Predictably, mayhem ensues. The case of the fictitious Harry Benson indeed has some similarities to the case of Thomas R, but so would many of Dr. Mark’s other patients, who had been evaluated and treated with deep brain recordings and stimulation of the amygdalas. I do not know who won the case or what settlement was reached. But careful review of the case reveals that for 14 years, before his psychosurgery, which entailed only stimulation (DBS) but not ablation of his amygdala, Thomas R, the once promising, “brilliant engineer” had become a man with an explosive temper, a case of dangerous, sociopathic incapacitation, unprovoked violence, and “pathologic aggression” directed against people around him, including his wife and family.[20,22,30] I have been told that in 1974 a block grant that had been extended by the Department of Justice for psychosurgical research to Drs. Mark and Ervin was rescinded. That was the end of brain research and evaluation of patients with abnormal brains and seizures associated with pathological aggression. For all practical purposes, it was the end of psychosurgery, except for the notable exception of Dr. Thomas Ballantine and stereotactic cingulotomy, whose work was related in of this historical review. And so by the time I had completed my undergraduate studies in Columbia at USC and had ascended the academic ladder to senior medical student at the Medical University of South Carolina (MUSC) in the charming southern city of Charleston, things had changed dramatically in the field of psychosurgery (which had so much attracted my curiosity and interest). In fact, the little book I used as a medical extern in neurological surgery in 1976, Dr. Sean Mullan’s Essentials of Neurosurgery (1964), had only two brief paragraphs dedicated to “psychosurgery” and the introductory sentence read, “This [psychosurgery] has ceased but was popular a decade ago.”[25]
ADVANCES IN STEREOTACTIC NEUROSURGERY (c. 1970-2000)
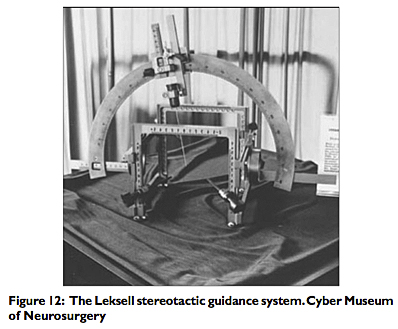
The National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research (1974-1978) eventually produced the Belmont Report that found that psychosurgery had provided and could provide meaningful benefits to many patients with neuropsychiatric disorders, but the pall had been cast on psychosurgery and the enthusiasm had been dampened in the antiestablishment era of the late 1960s and early 1970s, and as we have explained, neurosurgeons no longer wanted to trifle with psychosurgery and its associated political, social, and legal dangers.[31] In fact, critics of psychosurgery intended the National Commission to completely ban psychosurgery, instead the Belmont Report concluded that psychosurgery could provide “meaningful benefits to many patients with acceptable risks and should not be abolished outright.”[27] Model guidelines were established for informed consent and medical research. Nevertheless, the practice of psychosurgery declined dramatically after 1974. New procedures were developed in the context of “minimalist” functional neurosurgery and more precise stereotactic techniques using radiographic imaging.[27] The Swedish neurosurgeon Dr. Lars Leksell had introduced stereotactic radiosurgery in 1951 for more precise and localized irradiation of tissue ablation. He continued his groundbreaking work, and by 1968 he had developed the Leksell Stereotactic Guidance System, which he continued to improve through the 1980s [Figure 12].[18] A great breakthrough also occurred in neuroradiology with the invention of the EMI computerized tomography (CT) scanner, which was installed in the U.S. in 1973. By 1978 the concept of precise translation of imaging techniques to neurosurgical procedures, CT-stereotactic guided techniques, were also put into practice in the operating rooms.
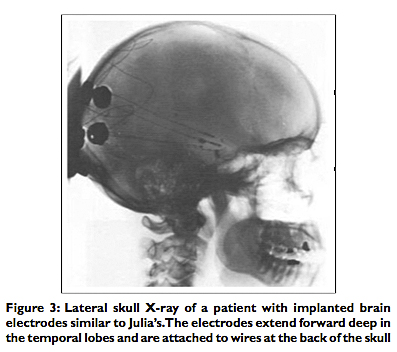
By the 1980s various neurosurgical groups in the U.S. were using the latest, imaged-guided Brown–Roberts–Wells (BRW) stereotactic system for the treatment of chronic pain and progressive movement disorders, particularly Parkinson’s disease. Magnetic resonance imaging (MRI) was developed in the 1980s, providing images with superlatively enhanced anatomic detail. In the 1990s, positron emission tomography (PET scan) allowed functional neural imaging detecting changes in glucose metabolism and cerebral blood flow. These advances permitted studies in psychiatric disorders, such as schizophrenia, major depressions, incapacitating obsessive–compulsive disorders (OCDs), and even antisocial personality disorders (ASPDs). PET scans can measure glucose metabolism rate and cerebral blood flow in different parts of the brain. Different patterns are reflected in different color images for normal controls and contrasted with those of patients with severe mental illnesses, such as schizophrenia and major clinical depression [Figures 13 and 14]. PET scan studies have also shown improved metabolic activity with successful pharmacotherapy.
Most stereotactic and functional neurosurgery since the 1980s has been directed to the management and neuromodulation of tone and movement disorders and the amelioration of chronic pain. Implantation of electrodes in the thalamus and basal ganglia has been followed by radiofrequency lesions or DBS in the surgical management of Parkinsonian and essential tremor. Obsessive-compulsive disorders (OCDs), which affect 2% of the population, can be a detrimental illness, and in 7% of patients, it’s refractory to conventional treatment with behavioral or pharmacotherapy. In Europe, investigators have found DBS to be helpful in alleviating some of the symptoms of OCD, and the CNS centers implicated in this condition are the nucleus accumbus and the connections between the ventral internal capsule and the amygdala, dorsomedial thalamus, and the prefrontal and orbitofrontal cortex. Thalamic DBS has been used in treatment of Gilles de la Tourette syndrome. Animal studies suggest that posttraumatic stress disorders (PTSD) associated with hyperarousal and severe emotional or social dysfunction may be alleviated by stimulation of the amygdala.[27]
VIOLENCE AND THE BRAIN IN THE 21ST CENTURY
Numerous studies in the past several decades have shown that psychopaths and other violent criminals have abnormal brain structures. Moreover, a small percentage of repeat offenders commit the vast majority of violent crimes in America. Following the tragic bombing and shooting incident in July 2011 in which Anders Behring Breivik, a Norwegian sociopath, massacred 77 people on an island near Oslo, Norway, interest was aroused to investigate why certain frustrated individuals seemingly explode, when responding to perceived threats or even without any provocation, to commit such atrocities.
Consider the 2012 report of researchers at King’s College London’s Institute of Psychiatry, who studied the brains of 44 violent adult male offenders in Britain. These men had already been diagnosed with anti-social personality disorders (ASPDs). Men diagnosed with ASPD characteristically react aggressively to frustration or perceived threats, lack emotion, such as the capability for embarrassment or to feel guilt, and in other psychological studies have been found to lack empathy or moral restraint. In this study, the crimes they had committed included murder, rape, attempted murder and grievous bodily harm. Of the 44 men scanned with magnetic resonance imaging (MRI), 17 met the diagnosis for ASPD plus “psychopathy,” and 27 did not. The brains of 22 normal men (controls) were also scanned. The results revealed that the brain of psychopaths had “significantly less grey matter in the anterior rostral prefrontal cortex and temporal poles” than the brains of the nonpsychopathic offenders and nonoffenders controls.[17] Very likely many of these male offenders have ASPD or are overt psychopaths. The British investigators added, that in England and Wales 50% of male prisoners meet diagnostic criteria for ASPD, and a review of studies covering 23,000 prisoners from 62 countries conducted in 2002 also concluded that 47% had ASPD.[17]
At the farther edge of neurological research, investigators have found a link between violent criminals and neuroradiographic abnormalities. Dr. Gerhard Roth, Professor of Neurology at the University of Bremen, Germany, conducted a study of violent convicted offenders and found on CT scan abnormal areas in the lower prefrontal cortex. The study consisted of showing short films and measuring the offenders’ brain activity. According to Roth, “Whenever there were brutal and squalid scenes, the subjects showed no emotions. In the areas of the brain where we create compassion and sorrow, nothing happened.”[16]
Likewise, Dr. Kent Kiehl, Associate Professor of Psychology at the University of New Mexico, conducted a study on “psychopathy, a personality disorder characterized by a pattern of disregard for the rights of others and the rules of society.” Kiehl used a mobile MRI to study 2000 inmate volunteers, including 200 women offenders and 250 juvenile delinquents. Kiehl found he could predict “psychopathy” using MRI images because of variability in gray matter density, which is linked to the MAOA gene in violent behavior. Adult psychopaths experienced recidivism rates of 60% and juvenile delinquents, 68%. Positive reinforcement therapy was found to be successful in young offenders only, and at a rate of only 50%.[24]
Kiehl’s study concluded by pointing out the high rate of incarceration of violent individuals in the U.S. and the astronomical cost it entails, approaching $2.3 trillion per year, about the same as the annual health care costs of the U.S.[24] The predictions of Dr. Vernon Mark, 40 years ago, it seems, have come to pass, and the problem of societal violence persists, and in some parameters has worsened on a global scale. Accumulating criminologic research, both in the United Kingdom and the United States over the years, attest that most violent crimes are committed by a small group of persistent criminals. In America, police and Federal Bureau of Investigation (FBI) statistics reveal that 75% of all violent crime is committed by 6% of hardened criminals and repeat offenders. Among these felons, murderers have a prior criminal history of at least 6 years with four felony arrests in their record before they finally commit murder.[6] Perhaps many of these murders could be prevented either by tougher criminal justice enforcement, or more humanely by studying medically selected offenders in specialized neurobiological research following the strict guidelines and informed consent rules established by the U.S. government in 1978.[31]
There is no unanimity on this subject, particularly brain localization and specific genetic markers for violence, but most neurosurgeons and neuroscientists have known, and still agree, that brain disease, such as infection, tumors and congenital abnormalities, may result in mental illness and do affect behavior, and in some cases criminal behavior. Yet, we must keep in mind the vast majority of the mentally ill are not violent, and most violent criminals, according to the present state of medical knowledge, are not insane but are repeat offenders, who take calculated risks when they decide to commit crimes.
CONCLUSION
I continue to believe that for the foreseeable future, violent individuals, who commit crimes but have no discernible brain neuropathology, should be managed conventionally, prosecuted by the criminal justice system according to the law. Our modern society, not even in democratic self-governance, to say nothing of authoritarian systems, has not advanced in ethical or moral wisdom to deal with the problems emanating from the technical and social “progress” of the age. Human violence and aggression persist, reminding us daily that civilization is a step away, perhaps only a generation away, from barbarism.
Criminal repeat offenders, on the other hand, who during medical examination are shown to have neuropathology discernible by the current state of medical knowledge, should, after the appropriate informed consent, be further evaluated and treated by qualified medical and nursing personnel trained in the management of “psychopathy.” Their management should include the usual treatments, for example, removal of brain tumors, control of seizure disorders with anticonvulsants, etc., as well as the administration of psychotropic drugs, ECT, and functional neurosurgery for their associated psychopathy in private facilities by private and academic physicians, but not government doctors or facilities. Government guidelines have been available since 1978 and seldom utilized for fear of bureaucratic red tape, legal repercussions, and the political and social zeitgeist of the times.
The state, though, still has a role; it can make sure the law is complied with, that the guidelines and amendments set by physicians are followed, that medical ethics (i.e., the individual-based ethics of Hippocrates) are observed,[1,7-10] but the state should not ideally be directly involved with funding institutions, medical personnel, or managing programs. Management should be left entirely in private hands, as the situation existed a century ago, when medical research took incredibly gigantic steps in scientific advancement in the hands of individual innovators and researchers with private funding and institutions. It is my belief that after a public education campaign, philanthropic individuals and institutions would step forward with private endowments to fund such a humanitarian endeavor. Still others may be propelled by tax incentives, as is the case with so many other beneficial activities encouraged in the public interest, such as other types of medical research and scholarship grants in higher education. Needless to say, all of my suggestions and considerations must be carefully considered by the general public and policy makers either before being implemented or more likely being dismissed outright.
The understandable concern is that if the state became a third-party payer in this endeavor, it would seek to control it, and in the process pervert medical ethics in the context of financial or political considerations. Once the state enters the equation, it would, if history is any guide, tilt the balance, not on behalf of the individual patient’s interest, but in its own budgetary or political interest. And so, were this process to go forward, the physicians must guard the interest of the “criminally insane” patient first, and the collective benefit to society, second. History forbids it otherwise.
Participating physicians, surgeons, and researchers must be very careful and remember what has been written and restated elsewhere. Namely, the lessons of history sagaciously reveal wherever the government has sought to alter medical ethics and control medical care, the results have been as perverse as they have been disastrous. In the 20th century both in the communist Soviet Union and fascist Nazi Germany, medicine regressed after these authoritarian systems corrupted the ethics of the medical profession and forced it to descend to unprecedented barbarism. The Soviet psychiatrists and Nazi doctor’s dark descent into barbarism was a product of physicians willingly cooperating with the totalitarian state, purportedly in the name of the “collective good,” at the expense of their individual patients.[8-10]
POSTSCRIPT
I performed my neurosurgical residency at Emory University in the early 1980s, but I did not train in my first neurosurgical attraction, psychosurgery, or even functional neurosurgery, except for a limited exposure to stereotaxis under the attending neurosurgeon at the Veteran’s Administration Hospital, my friend, Dr. Roy Bakay, who was in charge of functional neurosurgery and performed stereotactic surgery exclusively for movement disorders in the mid-1980s in Atlanta. My interest had switched to other areas of neurosurgery, such as the use of the CO2 laser in the treatment of brain tumors, EC-IC microvascular procedures, the study and treatment of the Chiari malformations, and the ubiquitous spinal surgeries. Psychosurgery was not done anymore, and in retrospect, even while I was still attending college and medical school, my conservative-libertarian leanings came to be in conflict with the theory as well as the wisdom of the state funding and immersing itself in new programs, to say nothing of sponsoring procedures that, although personally intriguing for me, nevertheless, could be misused.
In summation, my ambivalence remains regarding the ethics and potential abuse of psychosurgery. Presently, I oppose the use of psychosurgery in the treatment of psychopaths with “normal” brains in state-sponsored programs, but I believe that with today’s technology and with the federal guidelines still in place, it could be of benefit to society to encourage the medical profession, particularly neurologists and psychiatrists, to resume the study and investigation of patients afflicted with criminal rage, unprovoked fits of violence, and “pathological aggression,” not responding to the conventional measures (i.e., psychotherapy, rehabilitation, and drug therapy). Those patients selected because of discernable structural or electrophysiological abnormalities and established neuropathology should be considered potential candidates for referral to specialized research and treatment centers. Such centers that have opted to resume medical investigation of “psychopathy” and have established comprehensive treatments, including functional neurosurgery, should be allowed to do so in private institutions. The alternative is to continue the cycle of repeated incarcerations and futile hospitalizations with the inappropriate releases we have seen through the revolving doors in both the criminal justice and mental health systems, tragically for many people, who really harbor brain pathologies that may be amenable to treatment, and their victims.
Read Part 1 of this series: Violence, mental illness, and the brain — A brief history of psychosurgery: Part 1 — From trephination to lobotomy
Read Part 2 of this series: Violence, mental illness, and the brain — A brief history of psychosurgery: Part 2 — From the limbic system and cingulotomy to deep brain stimulation
REFERENCES
1. Arnett JC. . Medical Sentinel 2001; 6:63-65. [Last accessed on 6 Mar 2013].
2. Ballantine HT Jr, Giriunas IE. Advances in psychiatric surgery In: Rasmussen T,
Marino R, editors. Functional Neurosurgery. New York: Raven Press; 1979, p. 155-64.
3. Cannon WB. Bodily Changes in Pain, Hunger, Fear and Rage. New York: Appleton-Century-Crofts; 1920.
4. Delgado JM. . New York: Harper and Row; 1986. [Last accessed on 2013 Mar 1].
5. Delgado JM, Mark V, Sweet W, Ervin F, Weiss G, Bach-Y-Rita G, et al. Intracerebral radio stimulation and recording in completely free patients. J Nerv Ment Dis 1968;147:329-40.
6. Faria MA Jr. . Medical Sentinel 2001;6:14-18. [Last accessed on 2013 Mar 6].
7. Faria MA Jr. . Medical Sentinel 1998;3:19-24. [Last accessed on 2013 Mar 6].
8. Faria MA Jr. . West J Med 2000;172:224-225. [Last accessed on 2013 Mar 6].
9. Faria MA Jr. . HaciendaPublishing.com, October 24, 2012. [Last accessed on 2013 Mar 6 ].
10. Faria MA Jr. . Medical Sentinel 1998;3:79-83. [Last accessed on 2013 Mar 6].
11. Gilman S, Newman SW. Manter and Gatz’s Essentials of Clinical Neuroanatomy and Neurophysiology. 8th ed. Philadelphia: F. A. Davis Co.; 1992, p. 207-61.
12. Gonzalez ER. Psychosurgery waiting to make a comeback? JAMA 1980;244:2245-51.
13. Harlow HF. The development of affectional patterns in infant monkeys. In: Foss BM, editor. Determinants of Infant Behavior. London: Methuen; 1961, p. 75-88.
14. Hitchcock ER, Ballantine HT, Meyerson BA, editors. Modern Concepts in Psychiatric Surgery. New York: Elsevier/North Holland Biomedical Press; 1979, p. 111-27.
15. Horgan J. . Scientific American 2005;293:22-73. [Last accessed on 2013 Mar 1].
16. Kaplan JA. Fox News, February 7, 2013. [Last accessed on 2013 Mar 6].
17. Kelland K. . Reuters, London, May 7, 2012. [Last accessed on 2013 Mar 6].
18. Leksell L. Stereotactic radiosurgery. J Neurol Neurosurg Psychiatry 1983;46:797-803.
19. Lorenz K. On Aggression. New York: Harcourt, Brace and World; 1966.
20. Mark VH, Ervin FR. Violence and the Brain. New York: Harper and Row; 1970, p. 1-174.
21. Mark VH, Ervin FR. Violence and the Brain. New York: Harper and Row; 1970, p. 111.
22. Mark VH, Ervin FR. Violence and the Brain. New York: Harper and Row; 1970, p. 92-110, 172-175.
23. Montagu MF. Man and Aggression. New York: Oxford University Press; 1968.
24. Mooney A. . Duke University Research blog, April 23, 2012. [Last accessed on 2013 Mar 6].
25. Mullan S. Essentials of Neurosurgery – For Students and Practitioners. New York: Springer Publishing Company; 1964, p. 228.
26. Penfi eld W, Roberts L. Speech and Brain Mechanisms. New York: Atheneum; 1974.
27. Robison RA, Taghva A, Liu CY, Apuzzo ML. Surgery of the mind, mood and conscious state: An idea in evolution. World Neurosurg 2012;77:662-86.
28. Skinner BF. . New York: Alfred A. Knopf, Inc.; 1971. [Last accessed on 2013 Mar 12].
29. Sweet WH, Obrador S, Martin-Rodriguez JG, editors. Neurosurgical Treatment in Psychiatry, Pain, Epilepsy. Baltimore: University Park Press; 1977, p. 451-62.
30. $2-million “Terminal Man” suit under way. American Medical News, February 2, 1979, p. 1, 3.
31. United States Department of Health, Education and Welfare: Determination of the secretary regarding the recommendations on psychosurgery of the National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. Fed Regist 1978;43:53241-4.
32. Wilson H. Most of the time. MSN UK, December 24, 2011. [Last accessed on 2013 Mar 6].
Article written by: Dr. Miguel Faria
Miguel A. Faria, Jr., M.D. is Clinical Professor of Surgery (Neurosurgery, ret.) and Adjunct Professor of Medical History (ret.) Mercer University School of Medicine. He is an Associate Editor in Chief and a World Affairs Editor of Surgical Neurology International (SNI), and an Ex-member of the Injury Research Grant Review Committee of the Centers for Disease Control and Prevention (CDC). 2002-05; Former Editor-in-Chief of the Medical Sentinel (1996-2002), Editor Emeritus, the Association of American Physicians and Surgeons (AAPS); Author, Vandals at the Gates of Medicine (1995); Medical Warrior: Fighting Corporate Socialized Medicine (1997); and Cuba in Revolution: Escape From a Lost Paradise (2002).
This article was originally published in Surgical Neurology International and may be cited as: Faria MA. Violence, mental illness, and the brain — A brief history of psychosurgery: Part 3 — From deep brain stimulation to amygdalotomy for violent behavior, seizures, and pathological aggression in humans. Surg Neurol Int 2013;4(1):91. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3740620/
Available in this website: https://haciendapublishing.com/violence-mental-illness-and-the-brain-a-brief-history-of-psychosurgery-part-3-from-deep-brain-stimulation-to-amygdalotomy-for-violent-behavior-seizures-and-pathological-aggres/
Copyright © 2013 Miguel A. Faria, Jr., MD