- Articles
Violence, mental illness, and the brain — A brief history of psychosurgery: Part 1 — From trephination to lobotomy
Abstract — Psychosurgery was developed early in human prehistory (trephination) as a need perhaps to alter aberrant behavior and treat mental illness. The “American Crowbar Case” provided an impetus to study the brain and human behavior. The frontal lobe syndrome was avidly studied. Frontal lobotomy was developed in the 1930s for the treatment of mental illness and to solve the pressing problem of overcrowding in mental institutions in an era when no other forms of effective treatment were available. Lobotomy popularized by Dr. Walter Freeman reached a zenith in the 1940s, only to come into disrepute in the late 1950s. Other forms of therapy were needed and psychosurgery evolved into stereotactic functional neurosurgery. A history of these developments up to the 21st century will be related in this three-part historical review article, exclusively researched and written for the readers of Surgical Neurology International (SNI).
TREPHINATION, SHAMANS, AND MENTAL ILLNESS
Trephination (or trepanation) of the human skull is the oldest documented surgical procedure performed by man. Trephined skulls have been found from the Old World of Europe and Asia to the New World, particularly Peru in South America, from the Neolithic age to the very dawn of history.[3,14,18] [Figures 1 and 2] We can speculate why this skull surgery was performed by shamans or witch doctors, but we cannot deny that a major reason may have been to alter human behavior — in a specialty, which in the mid 20th century came to be called psychosurgery!
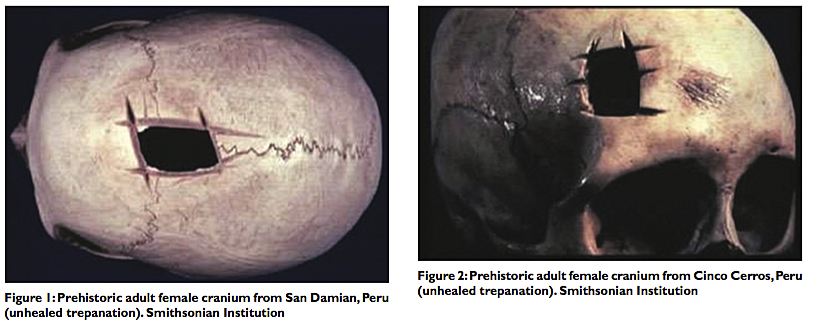
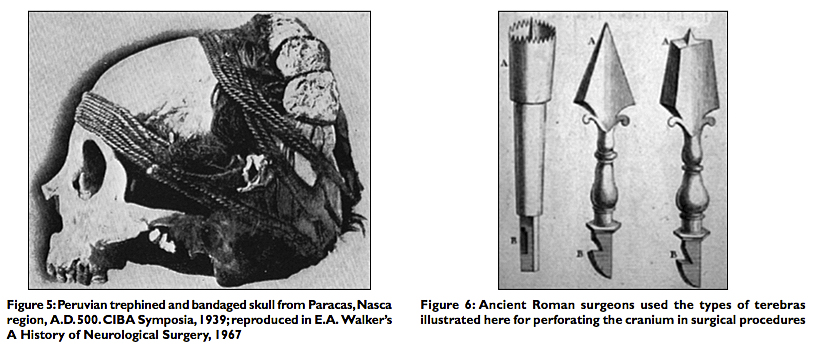
Surely we can surmise that intractable headaches, epilepsy, animistic possession by evil spirits, or mental illness, expressed by errant or abnormal behavior could have been indications for surgical intervention prescribed by the shaman of the late Stone or early Bronze Age. Dr. William Osler asserted, “[Trephination] was done for epilepsy, infantile convulsions, headache and various cerebral diseases believed to be caused by confined demons to whom the hole gave a ready method of escape.”[12] Once sanctioned by the tribe, the medicine man of the pre‑Inca, Peruvian civilization, could incise the scalp with his surgical knife and apply his tumi to the skull to ameliorate the headaches or release the evil spirits possessing the hapless tribesman [Figure 3]. And amazingly many of these patients of prehistoric times survived the surgery, at least for a time, as evidenced by bone healing at the edges of the trephined skulls that have been found by enterprising archeologists[3,14] [Figure 4]. We do not know if the patients’ clinical symptoms improved or if their behavior was modified after these prehistoric operations [Figure 5].
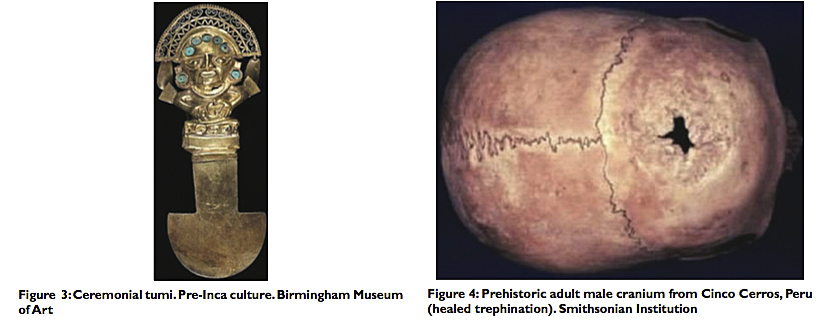
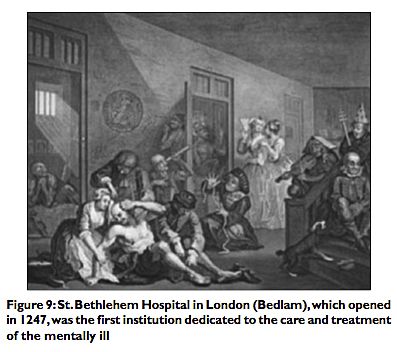
In ancient Greece and Rome, many medical instruments were designed to penetrate the skull. The Roman surgeons developed the terebra serrata, which was used to perforate the cranium by rolling the instrument between the surgeon’s hands [Figure 6]. Both the great physicians and surgeons, Celsus (c. 25 BC — c. AD 50) and Galen (c. AD 129 — c. AD 216) used these instruments. It is easy to see that the terebra was the forerunner of the manual burr hole and electric drill neurosurgeons use today for craniotomy procedures.
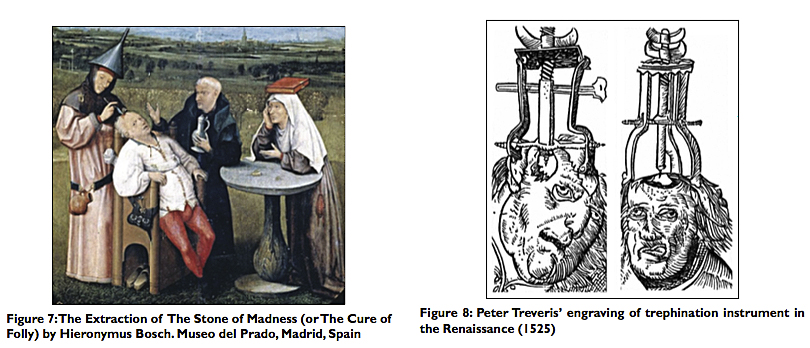
During the Middle Ages and the Renaissance, trepanation was performed not only for skull fractures but also for madness and epilepsy. There are telltale works of art from this period that bridge the gap between descriptive art and fanciful surgery. For example, we find the famous oil painting by Hieronymus Bosch (c. 1488-1516) that depicts “The Extraction of the Stone of Madness” [Figure 7]. Likewise, the triangular trephine instrument designed by Fabricius of Aquapendente (1537-1619) was subsequently used for opening and entering the skull; triangular trephines had already been modified for elevating depressed skull fractures. And thus, we find variations of the famous engraving by Peter Treveris (1525), illustrating surgical elevation of skull fractures, in many antiquarian medical textbooks[18] [Figure 8].
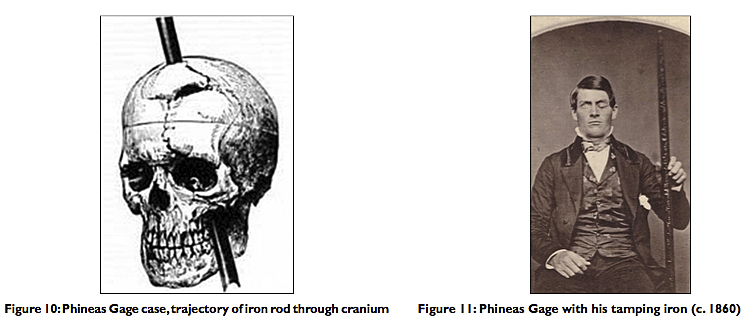
For most of man’s recorded history, the mentally ill have been treated as pariahs, ostracized by society and placed in crowded hospitals, or committed to insane asylums.[7] Criminals were dealt with swiftly and not always with justice or compassion. Despite the advent of more humane treatment in the late 19th century, hospitals for the mentally ill were poorly prepared to cope with the medical and social problems associated with mental illness and remained seriously overcrowded [Figure 9].
THE “AMERICAN CROWBAR CASE”
The early concept of cerebral localization (i.e., aphasia, hemiplegia, etc.) was derived first from the study of brain pathology, particularly cerebral tumors and operations for their removal;[9,16] and second, from the observation of dramatically altered behavior in a celebrated case of traumatic brain injury to the frontal lobe that has come to be called the “American Crowbar Case.”[11,19]
In 1848, Phineas P. Gage, a construction foreman at the Rutland and Burlington Railroad, was severely injured while helping construct a railway line near the town of Cavendish, Vermont. The premature explosion propelled a tamping iron — a long bar measuring 3 feet 7 inches in length and 1.25 inch in diameter – through Gage’s head. The 13.25 pound rod penetrated his left cheek, traversed the midline, the left frontal lobe, and exited the cranium just right of the midline near the intersection of the sagittal and coronal sutures [Figure 10].
The 25‑year‑old Gage survived, but the mental and behavioral changes noted by his doctor, friends, and co‑workers were significant. From being a motivated, energetic, capable, friendly, and conscientious worker, Gage changed dramatically into an obstinate, irreverent, irresponsible, socially uninhibited individual. These changes in personality would later be recognized as the frontal lobe syndrome. In the case of Gage, these changes were noted almost immediately after the injury. Close attention was paid to the case by Gage’s physician, Dr. John M. Harlow, not necessarily because of the personality changes but because the patient had survived such an extensive and serious injury and surgical ordeal.
The case received notoriety in the medical community when it was thoroughly described by Dr. Harlow 20 years later in an otherwise obscure medical journal. The doctor wrote: “Previous to his injury, although untrained in the schools, he possessed a well‑balanced mind, and was looked upon by those who knew him as a shrewd, smart businessman, very energetic and persistent in executing ll his plans of operation. In this regard his mind was radically changed, so decidedly that his friends and acquaintances said he was ‘no longer Gage.’”[8]
Dr. Harlow followed his patient’s travels across North and South America, and when Gage died in status epilepticus in 1860 near San Francisco, the doctor was able to retrieve the exhumed skull and tamping iron. Gage had continued to carry the rod wherever he went, his “constant companion” [Figure 11]. The ghastly items were donated to Harvard medical school’s Warren Anatomical Museum in 1868 after Dr. Harlow had finished his classic paper. The skull and tamping iron remain there to this day.
THE FRONTAL LOBE SYNDROME AND THE DEVELOPMENT OF LOBOTOMY (c. 1935)
The historic operation that we can arguably describe as the first psychosurgery procedure was performed by psychiatrist Dr. Gottlieb Burckhardt (1836-1907) in Switzerland in 1888. Burckhardt removed an area of cerebral cortex that he believed was responsible for his patient’s abnormal behavior. He followed this by performing selective resections mostly in the temporal and parietal lobes on six patients, areas in the lobes that Burckhardt considered responsible for his patients’ aggressive behavior and psychiatric disorder. His report was not well received by his colleagues and met with disapproval by the medical community. Subsequently, Burckhardt ceased work in this area.[15]
The Second International Neurologic Congress held in London in 1935 was a landmark plenary session for psychosurgery. American physiologist Dr. John F. Fulton (1899-1960) presented a momentous experiment in which two chimpanzees had bilateral resections of the prefrontal cortex. These operations were pioneering experiments in the field because the animals became “devoid of emotional expression” and were no longer capable of arousal of the “frustrational behavior” usually seen in these animals. The behavioral change was noted but the full implications were not. These findings would become very important decades later when social scientists in the 1970s noted that aggressive behavior and rage reaction were associated with low tolerance for frustration in individuals with sociopathic tendencies.[2]
This Congress was historic also because it was attended by personages who would leave marks in the history of psychosurgery, the neurosurgical treatment of mental disorders. Among the participants were two Portuguese neuroscientists: Dr. Antonio Egas Moniz (1874-1955), Professor of Neurology at the University of Lisbon, and his collaborator, the neurosurgeon Dr. Almeida Lima (1903-1985). They worked together in performing frontal leucotomies for psychiatric illnesses in the 1930s. In fact, Dr. Moniz’s efforts supported the work of physiologist John Fulton that frontal lobe ablation subdued the behavior of aggressive chimpanzees. Also attending this Congress was American neurologist Dr. Walter Freeman (1895-1972), who would soon leave a big imprint in the march of psychosurgery in the form of the frontal lobotomies.[13,15]
But there was more. Dr. R. M. Brickner described a patient with bilateral frontal lobectomies for excision of tumor. Postoperatively his patient showed a lack or restraint and social disinhibition, providing further evidence of the frontal lobe syndrome.[15]
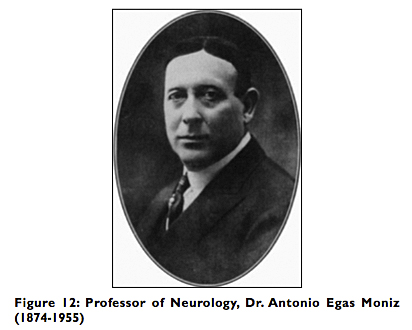
Frontal lobotomy, the sectioning of the prefrontal cortex, and leucotomy, the severing of the underlying white matter, for the treatment of mental disorders, reached a peak of popularity after World War II. But, as we have seen, development of this surgery began in the 1930s with the work of the celebrated Egas Moniz, who also made his mark in neuroradiology as the father of cerebral angiography [Figure 12]. Moniz and Lima performed their first frontal leucotomy in 1935. The following year Dr. Moniz presented a series of 20 patients, and by 1949 he had received the Nobel Prize for his pioneering work on frontal leucotomy in which, specifically, the white matter connections between the prefrontal cortex and the thalamus were sectioned to alleviate severe mental illness, including depression and schizophrenia in long‑term hospitalized patients.
It was at this time that a constellation of symptoms finally became associated with frontal lobe damage and removal — for example, distractibility, euphoria, apathy, lack of initiative, lack of restraint, and social disinhibition. Some of these symptoms were reminiscent of the personality changes noted by Dr. John M. Harlow in Phineas Gage nearly three quarters of a century
earlier.
THE PROBLEM OF MENTAL ILLNESS IN THE EARLY 20TH CENTURY
It must be remembered that this movement toward surgical intervention did not occur in a vacuum. It was engendered at a time when drug therapy was not available, and it involved mostly severely incapacitated patients for whom psychotherapy was ineffective or unavailable. Physicians, particularly psychiatrists and neurologists, those directly taking care of these unfortunate patients, were pushed against the wall to come up with effective therapy to modify abnormal psychiatric behavior and ameliorate mental suffering.
The problem of the increasing number of mentally ill patients for which no effective treatment was available, except for long‑term hospitalization and confinement, had been noted since the 19th century, and by the early 20th century the problem had reached gigantic proportions. Psychotropic drugs were not available until the 1950s, and in their absence, the only treatment options used in conjunction with long‑term hospitalization were physical restraint with the feared strait jackets, isolation in padded cells, etc., — i.e., conditions almost reminiscent of the notorious Bedlam Hospital of 19th century London.
Recently, Dr. R. A. Robison and colleagues summarized the socioeconomic context in which psychosurgery was advanced in the late 1930s by citing a 1937 report on the extent of institutionalization of the mentally ill in the United States: “There were more than 450,000 patients institutionalized in 477 asylums, with nearly one half of them hospitalized for five years or longer.” The cost in today’s dollars is estimated to have exceeded $24 billion.[15]
Psychotherapy, not to mention psychoanalysis, as proposed by Sigmund Freud (1856-1939), Carl Jung (1875-1961), and other prominent psychiatrists, was beyond the reach of most patients afflicted with psychiatric disorders until much later in the century. Advances in medicine and psychiatry in the latter part of the century would bring relief to untold millions but many problems even then would still persist.[2,5,15,17]
The leading lights of psychiatry at the turn of the century, Austrian psychoanalyst Sigmund Freud and German psychiatrist Emil Kraepelin (1856-1926) had conflicting approaches to mental illness. Freud recommended psychotherapy, often ineffective, almost always unfeasible in severely mentally ill patients, in which diseases ranged from tertiary syphilis and severe anxiety‑neuroses to agitated depression and schizophrenia. Kraepelin, in contrast, preferred more aggressive intervention with electroconvulsive therapy (ECT) and insulin shock therapy [Figure 13]. But what was to be done with patients who did not respond to these treatments, relapsed, or continued to pose a danger to themselves and others? That was the problem facing physicians at this time, particularly psychiatrists and neurologists. That also explains the fact the earliest “psychosurgeons” came disproportionally from these two specialties.
SURGERY OF THE FRONTAL LOBES — LEUCOTOMY AND LOBOTOMY (c. 1935-1955)
So it was in the mid 1930s under the circumstances of ineffectual treatments and hospital overcrowding that Moniz and Lima began to collaborate and carry out their work in Lisbon, Portugal. They developed the frontal leucotomy (or leukotomy), sectioning the white matter connections between the prefrontal cortex and the thalamus. First, they used alcohol injections; subsequently they introduced the leucotome and termed the procedure frontal leucotomy. They reported that their patients were more calm and manageable but their affect more blunted after the operations.
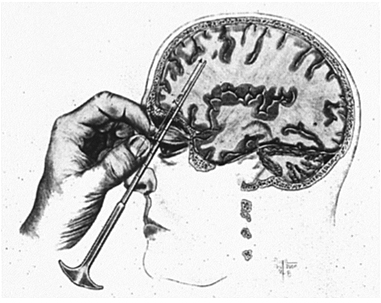
In the United States, Dr. James W. Watts (1904-1994), a neurosurgeon at George Washington University, was invited to collaborate with American neurologist and neuropathologist Dr. Walter Freeman (1895-1972) in developing the transorbital lobotomy in the early 1940s [Figure 14].
They performed the first frontal lobotomy in the U.S. in 1936 the same year Moniz presented his series of 20 patients from Portugal. With his knowledge of neuropathology, Freeman was able to visualize and analyze retrograde degeneration in postmortem examination of patients who had undergone the procedure and died later. He modified Moniz’s leucotome for better precision in targeting specific frontal lobe‑thalamic tracts. Patients with affective disorders had their leucotomy more anterior, whereas in those afflicted with more severe schizophrenic symptoms the lobotomy was more posterior.
In 1942, Freeman and Watts published the first edition of their classic monograph Psychosurgery and reported on 200 patients: 63% were improved; 23% had no improvement: and 14% were worsened or succumbed to their surgery.[6,15] That same year the Journal of the American Medical Association (JAMA) published an editorial supporting the basis for the procedure and the indications for lobotomies. Additional prestige for the operation was gained when Moniz received the Nobel Prize for Physiology or Medicine “for the discovery of the therapeutic value of leucotomy in certain psychoses” in 1949.[10]
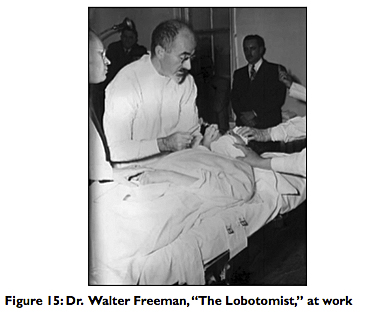
Freeman had used alcohol injections initially in some of his lobotomies, but he subsequently modified his procedure of transorbital leucotomy by using a modified ice‑pick instrument to traverse the roof of the orbit and enter the base of the skull. This was frequently done with local anesthesia or with sedation following ECT. The orbitoclast was then inserted to a depth of 7 cm at the base of the frontal lobes and swept 15° laterally.[15] Freeman hoped that physicians would use this simple technique to treat hospitalized patients widely [Figure 15]. Instead, the lack of sterile techniques and the crudity of the procedure disenchanted Watts, his neurosurgical associate, and also antagonized the neurosurgical establishment.[13] Many physicians became disappointed with the results, as some patients developed complications or died. But the majority of patients were improved, severe symptoms ameliorated, most families were gratified, and institutionalized patients became more manageable in the various institutions.[6,10,13,15]
Nevertheless, Freeman and Watts parted and went separate ways. Freeman became a relentless crusader and performed over 4000 lobotomies. Robison et al thus summarized the situation in a recent review article: “Despite resistance and reservations in the broader medical community, many psychiatrists and nonsurgical practitioners seized on the procedure as a new last resort for patients who lacked any effective alternate treatments.” Frontal lobotomy became a idely used procedure in the U.S., and an estimated 60,000 procedures were performed in the U.S. and in Europe between 1936 and 1956.[15]
By 1952, one of the pioneers of psychosurgery, the famed American physiologist John Fulton, was announcing the end of lobotomy and ushering in the beginning of stereotactic and functional neurosurgery because of improved precision and less cerebral tissue ablated. Chlorpromazine, which had been introduced in Europe in 1953, became available in the U.S. in 1955; haloperidol followed in 1967, and the drug therapy revolution was now also underway.[1] In 1971, Freeman published his long‑term follow up of 707 schizophrenics, 4-30 years after lobotomy. He reported that despite improvement in the majority, 73% were still hospitalized or at home in a “state of idle dependency.”[10]
SOCIOECONOMIC ASPECTS OF MENTAL ILLNESS AND INSTITUTIONALIZATION
The need to modify abnormal behavior and ameliorate mental suffering persists in our time. It has been estimated that 5 out of 10 cases of disability worldwide are attributable to mental disorders. And major depression heads the list of these psychiatric or psychological disorders with an incidence of 12-18% projected for the lifetime of the individual of the 21st century.[15] As many as one‑third of these afflicted patients have intractable depression unresponsive to antidepressant drugs or psychotherapy. We need not be reminded also that the vast majority of patients who commit suicide have suffered untreated depression or severe melancholia
unresponsive to treatment.
Despite psychotropic drugs, ECT, lobotomy, and psychosurgery, the societal problems posed by the prevalence of mental illness persist to this day. The steady institutionalization of the 1930s was followed by rapid deinstitutionalization in the 1970s. In 1963, U.S. President John F. Kennedy proposed a program for dealing with the persistent, unresolved problems of the mentally ill and the growing socioeconomic concerns of their long‑term institutionalization. Kennedy called for the formation of community mental health centers (CMHCs) funded by the federal government. Outpatient clinics replaced state hospitals and long‑term institutionalization. Over the next 17 years, the federal government funded 789 CMHCs, spending $20.3 billion in today’s dollars. “During those same years, the number of patients in state mental hospitals fell by three quarters — to 132,164 from 504,604,” laments Dr. E. Fuller Torrey, a noted psychiatrist and schizophrenia researcher. And he adds: “Those beds were closed down.”[17]
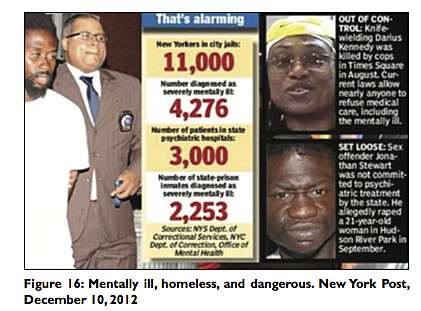
In the ensuing half century, these patients were discharged onto the streets of America, without family support and suffering from severe mental illness — including schizophrenia, bipolar and personality disorders, and criminal insanity. Half of them fare poorly.[2,4,5,17] Untreated mentally ill people in 2013, reports Dr. Torrey, are responsible for 10% of all homicides, constitute 20% of jail and prison inmates, and at least 30% of the homeless in the U.S.A. These homeless psychiatric patients spill over from the streets and city parks into the emergency rooms, libraries, and bus transit and train stations. Many of them join the ranks of the criminally insane and contribute significantly to the alarming statistics of crime and violence in America [Figure 16].
CONCLUSION
And so the problem of mental illness persists, influenced more by politics than mental health data and sound criminologic and sociologic scholarship.[4,5,17] Mental health deinstitutionalization poured the mentally ill onto the streets of America. The meek get preyed upon; the violent commit petty or serious crimes. Nevertheless, it should be pointed out that most mentally ill individuals are not violent but in need of medical care, compassion, and humanitarian assistance [Figure 17].
The social sciences in general and psychiatry in particular, despite the continued technological advances of our computer age, have not been able to keep up with the mounting psychological problems associated with this societal progress. Violent and criminal behavior, particularly when associated with repetitive, unprovoked aggression and low threshold rage reactions, also appear to be pernicious and recalcitrant elements of modern society, elements that have been difficult to explain and solve by our social scientists. In Part 2 — From the limbic system and cingulotomy to deep brain stimulation — we discuss new forms and methods of psychosurgery via stereotactic functional neurosurgery and advances in neuroscience. Part 3 will conclude this series.
REFERENCES
1. Brill H. Moderator. Chlorpromazine and Mental Health. Philadelphia: Lea and Febiger; 1955.
2. Coleman JC, Broen WE Jr. Abnormal Psychology and Modern Life. 4th ed. London: Scott, Foresman and Co.; 1972. p. 267‑403.
3. Faria MA Jr. . Macon, GA: Hacienda Publishing; 1995. p. 3‑11.
4. Faria MA Jr. . Surg Neurol Int 2013; 4:16. [Last accessed on 2013 Jan 29]
5. Fessenden F, Glaberson W, Goodstein L. They threaten, seethe and unhinge, then kill in quantity. The New York Times, April 9, 2000.
6. Freeman W, Watts JW. Psychosurgery. 2nd ed. Springfield, Illinois: Charles C. Thomas; 1952.
7. Haggard HW. The Doctor in History. New York: Dorset Press; 1989. p. 355‑70.
8. Harlow JM. Recovery from the passage of iron bar through the head. Publ Mass Med Soc 1868;2:327‑47.
9. Kirkpatrick DB. The first primary brain‑tumor operation. J Neurosurg 1984;61:809‑13.
10. Kucharski N. A History of frontal lobotomy in the United States, 1935‑1955. Neurosurgery 1984;14:765‑72.
11. Ordia JI. Neurologic function seven years after crowbar impalement of the brain. Surg Neurol 1989;32:152‑5.
12. Osler W. The Evolution of Modern Medicine. New Haven: Yale University Press; 1921. p. 6‑9.
13. PBS. . Video‑documentary, January 21, 2008. [Last accessed on 2013 Feb 27].
14. Rifkinson‑Mann S. Cranial surgery in Peru. Neurosurgery 1988;23:411‑6.
15. Robison RA, Taghva A, Liu CY, Apuzzo ML. Surgery of the mind, mood and conscious state: an idea in evolution. World Neurosurg 2012;77:662‑86.
16. Stone JL. Paul Broca and the first craniotomy. J Neurosurg 1991;75:154‑9.
17. Torrey EF. — JFK’s dream of replacing state mental hospitals with community mental health centers is now a hugely expensive nightmare. The Wall Street Journal, February 4, 2013. [Last accessed on 2013 Feb 4].
18. Walker AE, editor. A History of Neurological Surgery. New York: Hafner Publishing; 1967. p. 1‑22.
19. Walker AE, editor. A History of Neurological Surgery. New York: Hafner Publishing; 1967, p. 272‑85.
Article written by: Dr. Miguel Faria
Miguel A. Faria, Jr., M.D. is Clinical Professor of Surgery (Neurosurgery, ret.) and Adjunct Professor of Medical History (ret.) Mercer University School of Medicine. He is an Associate Editor in Chief and a World Affairs Editor of Surgical Neurology International (SNI), and an Ex-member of the Injury Research Grant Review Committee of the Centers for Disease Control and Prevention (CDC). 2002-05; Former Editor-in-Chief of the Medical Sentinel (1996-2002), Editor Emeritus, the Association of American Physicians and Surgeons (AAPS); Author, Vandals at the Gates of Medicine (1995); Medical Warrior: Fighting Corporate Socialized Medicine (1997); and Cuba in Revolution: Escape From a Lost Paradise (2002).
This article was originally published in Surgical Neurology International and may be cited as: Faria MA. Violence, mental illness, and the brain — A brief history of psychosurgery: Part 1 — From trephination to lobotomy. Surg Neurol Int 2013;4:49. Available from: http://surgicalneurologyint.com/surgicalint_articles/violence-mental-illness-and-the-brain-a-brief-history-of-psychosurgery-part-1-from-trephination-to-lobotomy/
Copyright © 2013 Miguel A. Faria, Jr., MD