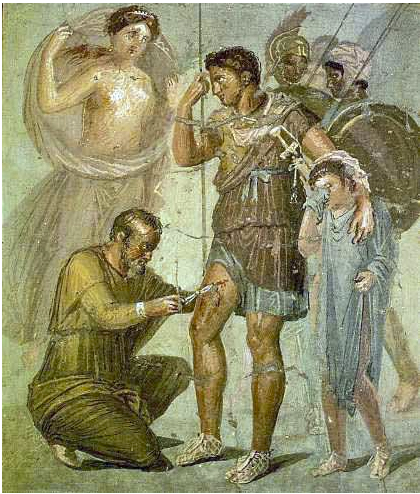
Another medical journey to ancient Rome and Roman medicine with medical historian Plinio Prioreschi, MD, PhD
This is the third volume of the monumental A History of Medicine series by the medical historian and classical scholar Plinio Prioreschi M.D., PhD.[1] A limited number of these books were published, and the reader would be fortunate to find copies of the tomes for less than $350 U.S. dollars. We have already reviewed Volume […]